Hereditary Hemorrhagic Telangiectasia, commonly abbreviated as HHT, is a rare genetic disorder that affects blood vessels throughout the body. This condition leads to abnormal connections between arteries and veins, resulting in weakened vessel walls that can cause bleeding and other complications. In this article, we will explore the intricacies of this disorder, including its causes, symptoms, and how individuals living with it can manage their health effectively.
Understanding the Disorder
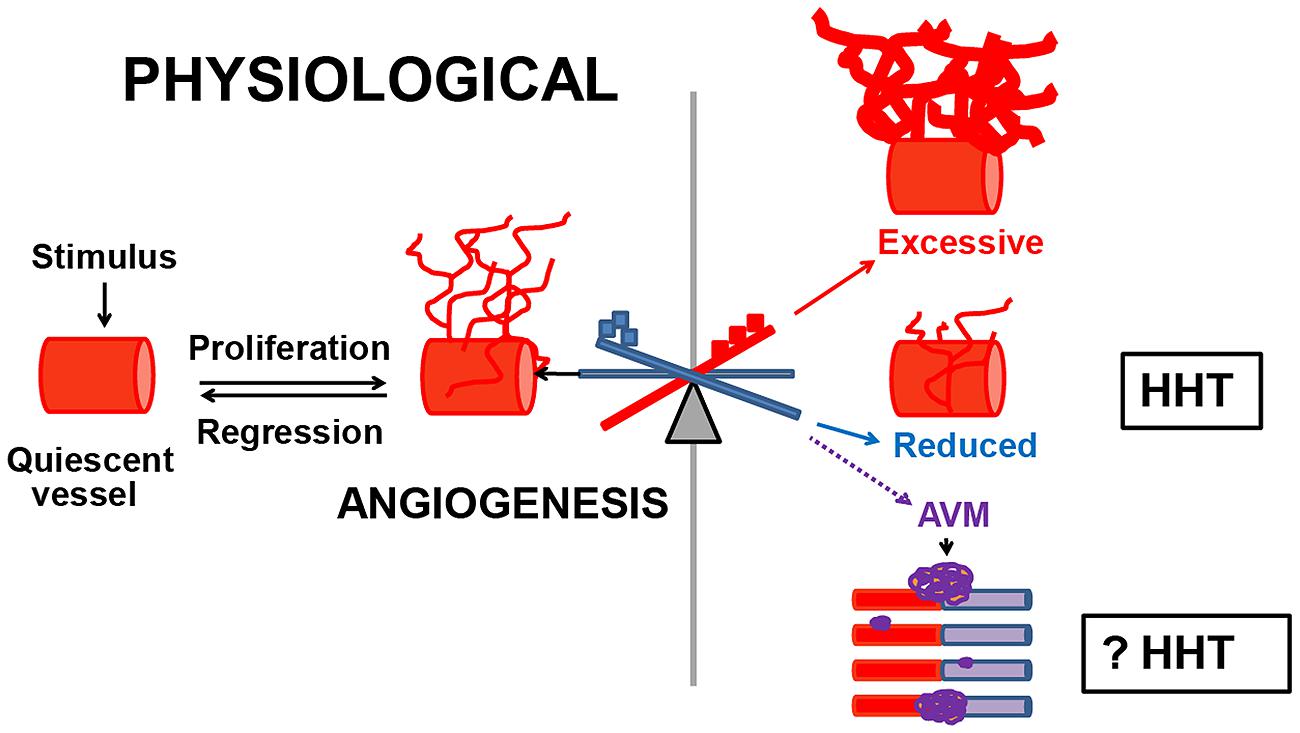
Hereditary Hemorrhagic Telangiectasia is a chronic condition that primarily impacts the vascular system. It is characterized by the development of abnormal blood vessels known as telangiectasias and arteriovenous malformations. These structural abnormalities disrupt normal blood flow, leading to a variety of symptoms and potential complications.
What Are Telangiectasias?
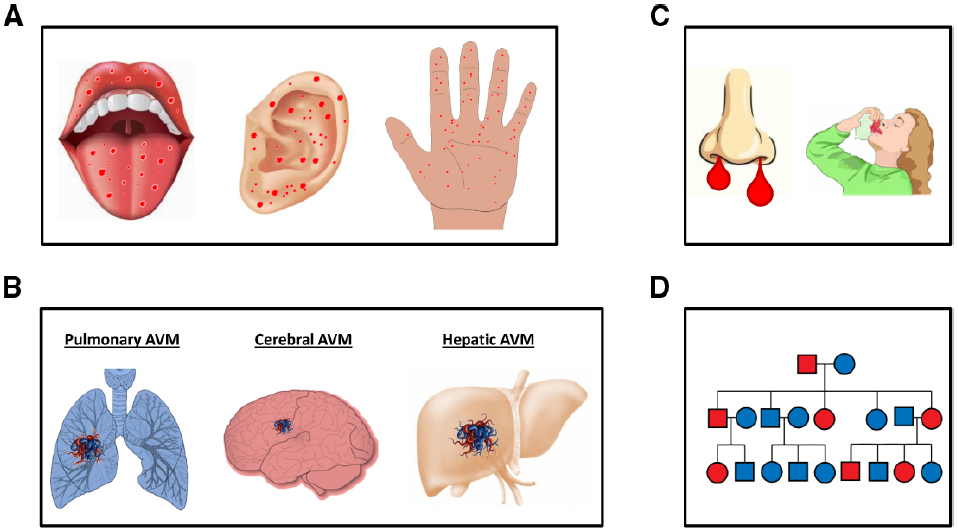
Telangiectasias are small, dilated blood vessels that appear near the surface of the skin or mucous membranes. They often look like tiny red or purple spots and are most commonly found on the face, lips, fingers, and inside the mouth or nose. While they may seem harmless, these abnormal vessels are prone to bleeding, which can lead to significant health challenges over time.
Arteriovenous Malformations Explained
Arteriovenous malformations are larger, more complex abnormal connections between arteries and veins. Unlike telangiectasias, these malformations are typically located deeper within the body, such as in the lungs, liver, brain, or gastrointestinal tract. Because they bypass the capillaries, arteriovenous malformations can interfere with oxygenation and nutrient delivery, posing serious risks to affected organs.
Causes of the Condition
The root cause of this vascular disorder lies in genetic mutations that are passed down through families. The condition follows an autosomal dominant inheritance pattern, meaning that only one copy of the mutated gene is needed for an individual to develop the disorder. If one parent carries the gene mutation, there is a 50 percent chance that their child will inherit it.
Genetic Mutations Involved
Several genes have been identified as contributors to this condition. The two most common culprits are the ENG gene and the ACVRL1 gene. These genes provide instructions for making proteins that play critical roles in the formation and maintenance of blood vessels. When mutations occur, the proteins are either missing or malfunctioning, leading to the characteristic vascular abnormalities seen in affected individuals.
Environmental Factors and Triggers
While the primary cause of the condition is genetic, certain environmental factors may exacerbate symptoms or trigger complications. For example, high altitudes, pregnancy, and hormonal changes can increase the likelihood of bleeding episodes. Additionally, activities that elevate blood pressure, such as heavy lifting or intense exercise, may also worsen symptoms in some cases.
Symptoms of the Disorder
The symptoms of this vascular condition can vary widely from person to person, even among members of the same family. Some individuals may experience mild symptoms, while others may face severe complications. Recognizing the signs early can help ensure timely diagnosis and treatment.
Recurrent Nosebleeds
One of the hallmark symptoms of this condition is frequent and spontaneous nosebleeds. These episodes can range from mild to severe and often begin during childhood. Over time, recurrent nosebleeds can lead to iron deficiency anemia due to chronic blood loss.
Telangiectasias on the Skin and Mucous Membranes
As mentioned earlier, telangiectasias are small, visible blood vessels that appear on the skin or mucous membranes. While they are not painful, they can cause cosmetic concerns and are prone to bleeding, especially if irritated.
Gastrointestinal Bleeding
- Bleeding in the gastrointestinal tract is another common symptom, particularly in older adults with the condition.
- This type of bleeding may present as black, tarry stools or vomiting blood, both of which require immediate medical attention.
- Over time, gastrointestinal bleeding can contribute to anemia and fatigue.
Complications from Arteriovenous Malformations
Arteriovenous malformations can lead to life-threatening complications depending on their location:
- Lungs: Malformations in the lungs can result in shortness of breath, low oxygen levels, and an increased risk of stroke due to blood clots traveling to the brain.
- Brain: When located in the brain, these malformations may cause headaches, seizures, or even hemorrhagic strokes.
- Liver: Liver involvement can lead to heart failure due to the increased workload placed on the heart as it pumps blood through malformed vessels.
Diagnosis and Screening
Diagnosing this vascular disorder can be challenging because its symptoms often overlap with those of other conditions. However, a combination of clinical evaluation, imaging studies, and genetic testing can help confirm the presence of the disease.
Clinical Criteria
Doctors often use a set of criteria known as the Curaçao criteria to diagnose the condition. These include:
- Recurrent nosebleeds
- Presence of telangiectasias
- Arteriovenous malformations detected through imaging
- A family history of the disorder
If a patient meets three or more of these criteria, the likelihood of having the condition is high.
Imaging Techniques
Advanced imaging techniques such as magnetic resonance imaging (MRI), computed tomography (CT) scans, and ultrasound are essential tools for identifying arteriovenous malformations. These tests allow doctors to pinpoint the location and severity of vascular abnormalities, guiding treatment decisions.
Genetic Testing
Genetic testing is particularly useful for confirming a diagnosis and identifying family members who may be at risk. By analyzing a sample of blood or saliva, scientists can detect mutations in the genes associated with the condition.
Management and Care
While there is no cure for this vascular disorder, various treatments and lifestyle modifications can help manage symptoms and prevent complications. A multidisciplinary approach involving specialists such as hematologists, pulmonologists, and gastroenterologists is often necessary to provide comprehensive care.
Treating Nosebleeds
For individuals experiencing frequent nosebleeds, several interventions may be recommended:
- Topical Treatments: Nasal sprays containing saline or estrogen can help reduce bleeding episodes.
- Laser Therapy: Laser treatments can seal off problematic blood vessels in the nasal passages.
- Surgical Options: In severe cases, procedures such as septal dermoplasty may be considered to address persistent bleeding.
Managing Anemia
Chronic blood loss from nosebleeds or gastrointestinal bleeding can lead to anemia, which is characterized by fatigue, weakness, and shortness of breath. Iron supplements and dietary changes are often prescribed to boost iron levels. In severe cases, blood transfusions may be necessary.
Addressing Arteriovenous Malformations
Treatment for arteriovenous malformations depends on their size, location, and the symptoms they cause. Options include:
- Embolization: This minimally invasive procedure involves blocking abnormal blood vessels using special materials delivered via a catheter.
- Surgery: Surgical removal may be required for large or symptomatic malformations that cannot be treated with embolization.
- Radiation Therapy: In some cases, radiation may be used to shrink arteriovenous malformations in sensitive areas like the brain.
Lifestyle Modifications
Making certain lifestyle adjustments can significantly improve quality of life for individuals with this condition:
- Dietary Changes: Consuming iron-rich foods and avoiding irritants like alcohol and spicy foods can help manage gastrointestinal symptoms.
- Avoiding Triggers: Steering clear of activities that raise blood pressure or stress the vascular system is advisable.
- Regular Monitoring: Routine check-ups and screenings are crucial for detecting new or worsening vascular abnormalities early.
Living with the Condition
Living with this vascular disorder requires resilience and proactive healthcare management. Support groups and educational resources can provide valuable guidance and emotional support for patients and their families. By staying informed and working closely with healthcare providers, individuals with the condition can lead fulfilling lives despite its challenges.