Heart block, also known as atrioventricular block, is a condition where the electrical signals that control the heartbeat are disrupted. This disruption can lead to an irregular heartbeat or even cause the heart to stop beating temporarily. Heart block is classified into different types based on its severity and location within the heart’s electrical system. In this article, we will explore the various types of heart block, their underlying causes, and the available treatments.
What Is Heart Block?
The heart relies on a complex electrical system to maintain a steady rhythm. This system ensures that the upper chambers (atria) and lower chambers (ventricles) of the heart contract in a coordinated manner. When there is an interruption in this electrical pathway, it results in a heart block. Depending on the extent of the disruption, heart block can range from mild to life-threatening.
How Does the Heart’s Electrical System Work?
- Sinoatrial Node: Often referred to as the natural pacemaker of the heart, this node generates electrical impulses that initiate each heartbeat.
- Atrioventricular Node: This node acts as a gateway, allowing electrical signals to pass from the atria to the ventricles.
- Bundle Branches and Purkinje Fibers: These structures carry the electrical signals through the ventricles, causing them to contract and pump blood.
When any part of this system malfunctions, it can result in a heart block.
Types of Heart Block
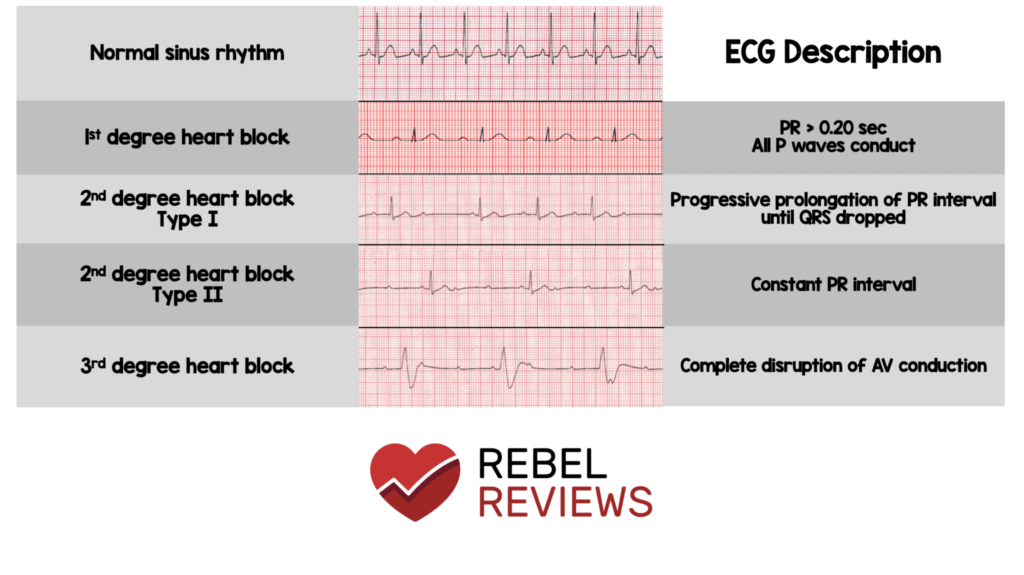
Heart block is categorized into three main types based on the degree of electrical signal disruption. Each type has distinct characteristics and implications for health.
First-Degree Heart Block
First-degree heart block occurs when the electrical signals are delayed as they pass through the atrioventricular node. However, all signals eventually reach the ventricles, so the heart continues to beat normally. People with this type of heart block often do not experience symptoms and may only discover the condition during routine medical tests.
- Symptoms: Typically asymptomatic.
- Cause: Can be caused by medications, electrolyte imbalances, or minor damage to the heart’s electrical system.
Second-Degree Heart Block
Second-degree heart block is further divided into two subtypes: Mobitz Type I and Mobitz Type II. In both cases, some electrical signals fail to reach the ventricles, leading to occasional missed heartbeats.
Mobitz Type I (Wenckebach)
In Mobitz Type I, the delay in electrical signals increases progressively until one signal fails to reach the ventricles. This type is usually less serious and may not require treatment unless symptoms develop.
- Symptoms: May include dizziness, fatigue, or palpitations.
- Cause: Often related to conditions like myocardial infarction or inflammation of the heart muscle.
Mobitz Type II
Mobitz Type II is more severe than Type I because the electrical signals are intermittently blocked without warning. This can lead to significant drops in heart rate and requires immediate medical attention.
- Symptoms: Fainting, chest pain, or shortness of breath.
- Cause: Often associated with structural damage to the heart, such as scarring from a previous heart attack.
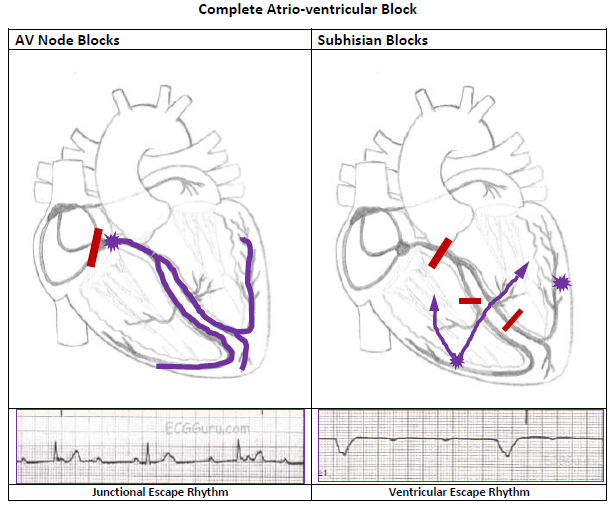
Third-Degree Heart Block
Third-degree heart block, also known as complete heart block, occurs when no electrical signals pass from the atria to the ventricles. As a result, the atria and ventricles beat independently of each other, leading to a dangerously slow heart rate. This type of heart block is considered a medical emergency.
- Symptoms: Severe fatigue, fainting, confusion, or even cardiac arrest.
- Cause: Can result from congenital defects, degenerative diseases, or severe damage to the heart’s electrical system.
Causes of Heart Block
Heart block can arise from a variety of factors, ranging from genetic predispositions to acquired conditions. Understanding the underlying causes can help in managing and preventing the condition.
Congenital Heart Block
Congenital heart block is present at birth and is often associated with autoimmune disorders in the mother, such as lupus. It can also occur due to structural abnormalities in the heart’s electrical system.
Acquired Heart Block
Acquired heart block develops later in life and is often linked to the following factors:
- Heart Disease: Conditions like coronary artery disease, heart attacks, or cardiomyopathy can damage the heart’s electrical pathways.
- Medications: Certain drugs, such as beta-blockers or calcium channel blockers, can interfere with electrical signals.
- Infections: Viral infections like Lyme disease can inflame the heart and disrupt its electrical system.
- Age-Related Changes: The natural aging process can lead to fibrosis or scarring of the heart’s conduction system.
Treatments for Heart Block
The treatment for heart block depends on its type and severity. While some cases may not require intervention, others necessitate immediate medical attention.
Monitoring and Lifestyle Changes
For first-degree heart block and mild cases of second-degree heart block, treatment may involve regular monitoring and lifestyle modifications. These include:
- Regular check-ups with a healthcare provider.
- Avoiding medications that exacerbate the condition.
- Maintaining a heart-healthy diet and exercise routine.
Pacemakers
For more severe cases, such as Mobitz Type II or third-degree heart block, a pacemaker is often required. A pacemaker is a small device implanted under the skin that helps regulate the heartbeat by sending electrical signals to the heart.
- Procedure: Pacemaker implantation is a minimally invasive surgery performed under local anesthesia.
- Benefits: Restores normal heart rhythm and improves quality of life.
Medications
In some cases, medications may be prescribed to manage symptoms or address underlying causes of heart block. These may include:
- Antiarrhythmic drugs to stabilize the heart rhythm.
- Medications to treat infections or reduce inflammation.
Emergency Interventions
For individuals experiencing third-degree heart block or severe symptoms, emergency interventions may be necessary. These can include:
- Temporary pacing using external devices until a permanent pacemaker can be implanted.
- Cardiopulmonary resuscitation in cases of cardiac arrest.
Living with Heart Block
While heart block can be a challenging condition to manage, many individuals live full and active lives with proper care. Regular follow-ups with healthcare providers, adherence to treatment plans, and awareness of potential symptoms are crucial for maintaining heart health.
Tips for Managing Heart Block
- Stay informed about your condition and treatment options.
- Report any new or worsening symptoms to your doctor immediately.
- Avoid activities that strain the heart, such as heavy lifting or extreme physical exertion.