A goiter, which refers to an abnormal enlargement of the thyroid gland, is a condition that can affect individuals across various age groups and demographics. While it may not always cause pain or immediate health concerns, understanding its underlying causes, symptoms, and treatment options is essential for maintaining overall well-being. In this article, we will delve into the intricacies of goiters, exploring what they are, why they occur, and how they can be managed effectively.
What Is a Goiter?
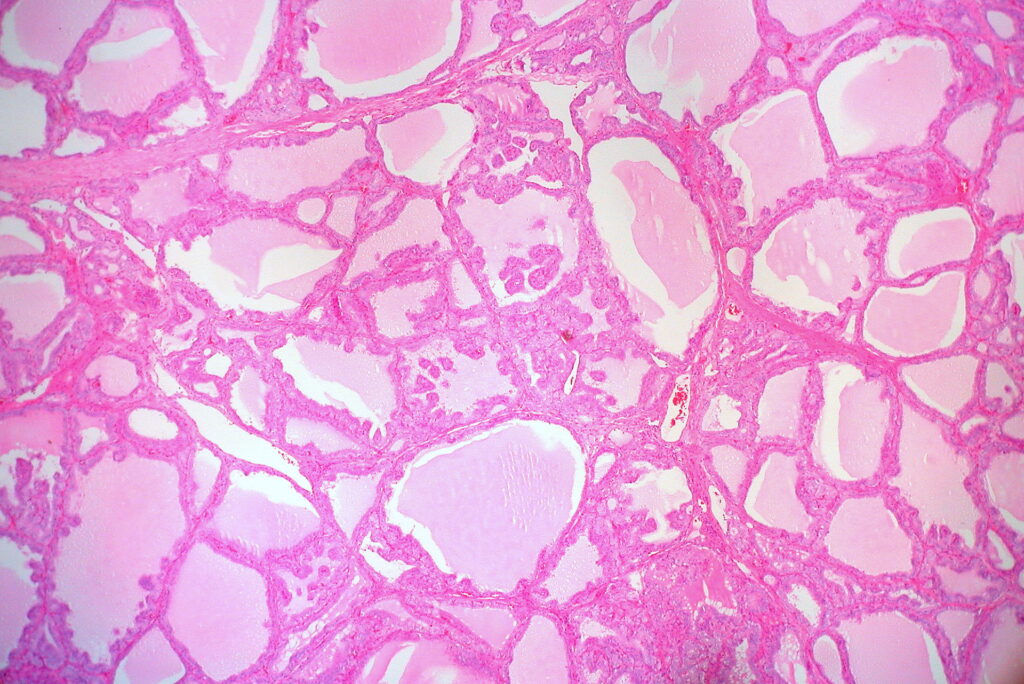
The thyroid gland, located at the base of the neck, plays a crucial role in regulating metabolism, energy production, and overall bodily functions by producing hormones. A goiter occurs when this gland becomes enlarged, often causing visible swelling in the neck. The size of a goiter can vary significantly, ranging from small and barely noticeable to large enough to interfere with breathing or swallowing.
It is important to note that a goiter itself is not a disease but rather a symptom of an underlying issue affecting the thyroid. This could include conditions such as iodine deficiency, autoimmune disorders, or hormonal imbalances.
Common Causes of Goiters
Several factors can contribute to the development of a goiter. Below, we explore some of the most common causes:
Iodine Deficiency
Iodine is an essential mineral required for the production of thyroid hormones. When the body does not receive adequate amounts of iodine through diet, the thyroid gland may enlarge in an attempt to compensate for the deficiency. This is one of the leading causes of goiters worldwide, particularly in regions where iodine-rich foods are scarce.
Autoimmune Disorders
Autoimmune conditions such as Graves’ disease and Hashimoto’s thyroiditis can also lead to goiters. In Graves’ disease, the immune system mistakenly stimulates the thyroid to produce excessive amounts of hormones, causing the gland to enlarge. Conversely, Hashimoto’s thyroiditis results in inflammation and reduced hormone production, prompting the gland to swell as it struggles to function properly.
Hormonal Imbalances
Pregnancy, menopause, and other life stages that involve significant hormonal changes can sometimes trigger the development of a goiter. For example, during pregnancy, the body requires increased levels of thyroid hormones, which may place additional strain on the thyroid gland.
Nodules and Cysts
In some cases, the presence of benign growths, such as nodules or cysts, can cause the thyroid gland to enlarge. These growths are typically harmless but may require monitoring to ensure they do not interfere with thyroid function or grow excessively large.
Medications and Environmental Factors
Certain medications, such as lithium, have been linked to thyroid dysfunction and goiter formation. Additionally, exposure to environmental toxins or radiation can increase the risk of developing a goiter.
Symptoms of a Goiter
The symptoms associated with a goiter can vary depending on its size and the underlying cause. Some individuals may experience no symptoms at all, while others may notice the following:
- A visible swelling or lump at the base of the neck
- Tightness or discomfort in the throat area
- Difficulty swallowing or breathing
- Hoarseness or changes in voice
- Coughing or wheezing
In cases where the goiter is caused by an overactive or underactive thyroid, additional symptoms may arise. For instance, hyperthyroidism (excessive hormone production) can lead to weight loss, rapid heartbeat, and anxiety, while hypothyroidism (insufficient hormone production) may result in fatigue, weight gain, and depression.
Diagnosing a Goiter
If a goiter is suspected, healthcare providers typically begin with a physical examination to assess the size and texture of the thyroid gland. They may also inquire about symptoms, medical history, and dietary habits to identify potential contributing factors.
To confirm the diagnosis and determine the underlying cause, several tests may be conducted, including:
- Blood Tests: These measure levels of thyroid hormones and thyroid-stimulating hormone to evaluate thyroid function.
- Ultrasound Imaging: This non-invasive procedure provides detailed images of the thyroid gland, helping to detect nodules, cysts, or other abnormalities.
- Fine-Needle Aspiration Biopsy: If nodules are present, a small sample of tissue may be extracted for analysis to rule out cancer.
- Radiological Scans: In some cases, radioactive iodine scans may be used to assess thyroid activity and identify areas of concern.
Treatment Options for Goiters
The treatment approach for a goiter depends on its size, symptoms, and underlying cause. Below are some of the most common treatment options:
Observation and Monitoring
For small, asymptomatic goiters that do not interfere with thyroid function, regular monitoring may be recommended. During this time, healthcare providers will track any changes in size or symptoms through periodic examinations and tests.
Dietary Adjustments
In cases where iodine deficiency is the primary cause, increasing dietary intake of iodine-rich foods such as seafood, dairy products, and iodized salt can help alleviate the condition. However, it is important to consult a healthcare provider before making significant dietary changes, as excessive iodine consumption can also harm thyroid function.
Medications
Medications may be prescribed to address specific underlying causes of a goiter. For example:
- Hormone Replacement Therapy: Individuals with hypothyroidism may benefit from synthetic thyroid hormones to restore balance and reduce gland enlargement.
- Anti-Thyroid Medications: For those with hyperthyroidism, drugs that inhibit hormone production may be used to manage symptoms and shrink the goiter.
Radiation Therapy
In certain cases, radioactive iodine therapy may be recommended to treat overactive thyroid glands. This procedure involves ingesting a small amount of radioactive iodine, which targets and destroys overactive thyroid cells, thereby reducing the size of the goiter.
Surgical Intervention
Surgery may be necessary for large goiters that cause significant discomfort, difficulty breathing or swallowing, or cosmetic concerns. During the procedure, part or all of the thyroid gland may be removed, depending on the severity of the condition. Post-surgery, patients may require lifelong hormone replacement therapy to maintain normal thyroid function.
Preventing Goiters
While not all goiters can be prevented, certain measures can reduce the risk of developing this condition:
- Maintain a balanced diet rich in iodine and other essential nutrients.
- Avoid excessive consumption of goitrogenic foods, such as soy products and cruciferous vegetables, which can interfere with thyroid function when consumed in large quantities.
- Undergo regular check-ups to monitor thyroid health, especially if there is a family history of thyroid disorders.
- Minimize exposure to environmental toxins and radiation whenever possible.
Living with a Goiter
For many individuals, living with a goiter involves managing symptoms and addressing the underlying cause. By working closely with healthcare providers and adhering to prescribed treatment plans, most people can lead healthy, fulfilling lives despite their condition. Support groups and educational resources can also provide valuable insights and emotional support for those navigating the challenges of thyroid health.