Folate deficiency, often abbreviated as FD, is a condition that occurs when the body lacks sufficient folate, a vital B vitamin. Folate plays an essential role in various bodily functions, including DNA synthesis, red blood cell production, and the proper functioning of the nervous system. Without adequate levels of this nutrient, individuals may experience a range of health issues that can significantly impact their quality of life. In this article, we will explore the causes, symptoms, diagnosis, and treatment options for this condition.
Understanding Folate and Its Importance
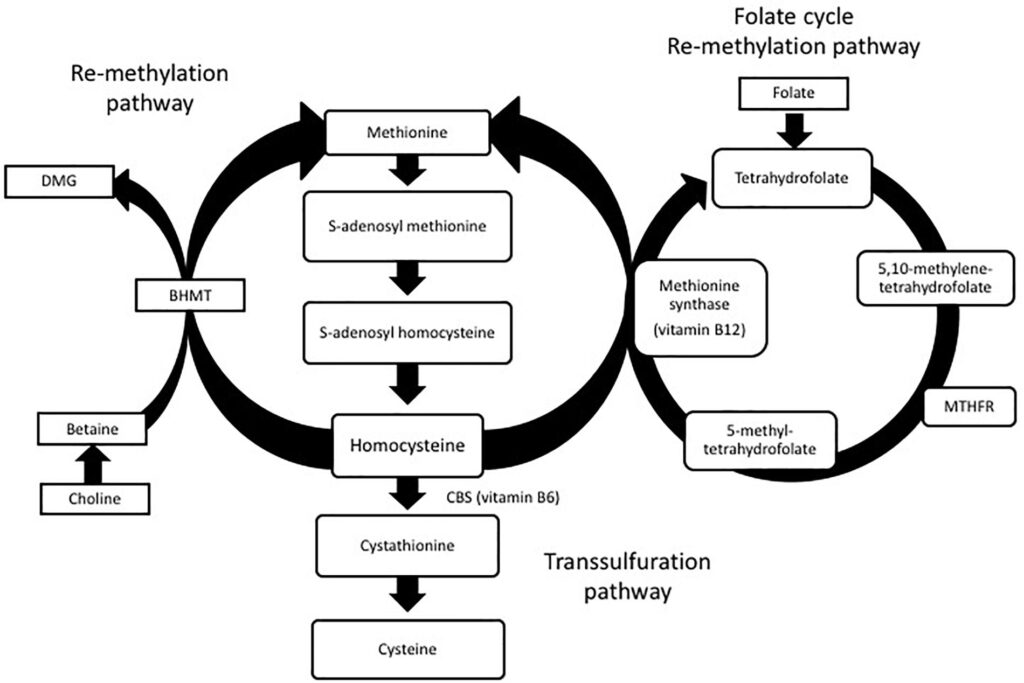
Folate, also known as vitamin B9, is a water-soluble vitamin that is naturally present in many foods. It is crucial for several biological processes, including the formation of genetic material like DNA and RNA, the production of red blood cells, and the metabolism of amino acids. Folate is especially important during periods of rapid growth, such as pregnancy and infancy, as it supports the development of the fetal brain and spinal cord.
When the body does not receive enough folate through diet or other means, it can lead to a deficiency. This deficiency can have serious consequences, particularly for pregnant women, as it increases the risk of neural tube defects in developing babies. Additionally, folate deficiency can contribute to anemia, fatigue, and other health complications.
Causes of Folate Deficiency
There are several potential causes of folate deficiency, ranging from dietary insufficiencies to medical conditions that interfere with folate absorption. Below are some of the most common causes:
- Inadequate Dietary Intake: A diet low in folate-rich foods, such as leafy green vegetables, fruits, and fortified grains, can lead to a deficiency. People who consume highly processed foods or follow restrictive diets may be at higher risk.
- Malabsorption Disorders: Certain medical conditions, such as celiac disease, Crohn’s disease, and inflammatory bowel disease, can impair the body’s ability to absorb folate from food.
- Increased Folate Requirements: Pregnant women, breastfeeding mothers, and individuals with chronic hemolytic anemia require higher levels of folate. If these needs are not met, a deficiency can develop.
- Medications: Some medications, such as methotrexate, phenytoin, and sulfasalazine, can interfere with folate metabolism or absorption, leading to a deficiency over time.
- Alcoholism: Excessive alcohol consumption can interfere with folate absorption and increase its excretion from the body, contributing to a deficiency.
- Genetic Factors: Rare genetic disorders, such as methylenetetrahydrofolate reductase deficiency, can affect how the body processes folate, increasing the risk of deficiency.
Symptoms of Folate Deficiency
The symptoms of folate deficiency can vary depending on the severity of the condition and the individual’s overall health. In mild cases, symptoms may be subtle or even absent, while severe deficiencies can lead to more pronounced signs. Common symptoms include:
- Fatigue: One of the earliest and most common symptoms, fatigue occurs because folate is essential for producing healthy red blood cells, which carry oxygen throughout the body.
- Pale Skin: A lack of folate can lead to a decrease in red blood cells, resulting in pale skin and mucous membranes.
- Mouth Sores and Tongue Swelling: Folate deficiency can cause inflammation of the tongue and the development of painful sores in the mouth.
- Gastrointestinal Issues: Symptoms such as diarrhea, nausea, and loss of appetite are often associated with folate deficiency.
- Irritability and Cognitive Impairment: Low levels of folate can affect brain function, leading to irritability, difficulty concentrating, and memory problems.
- Anemia: Folate deficiency can result in megaloblastic anemia, a condition characterized by the production of abnormally large and immature red blood cells.
Diagnosing Folate Deficiency
Diagnosing folate deficiency typically involves a combination of clinical evaluation, medical history review, and laboratory tests. Healthcare providers may suspect a deficiency based on the patient’s symptoms and risk factors, but confirmatory testing is necessary to make an accurate diagnosis.
Laboratory Tests
Several laboratory tests can help identify folate deficiency:
- Blood Tests: A complete blood count can reveal signs of anemia, such as low red blood cell counts or abnormal cell size. Additionally, serum folate levels can be measured to assess the amount of folate circulating in the blood.
- Red Blood Cell Folate Test: This test measures the amount of folate stored within red blood cells and provides a more accurate reflection of long-term folate status compared to serum folate levels.
- Homocysteine Levels: Elevated levels of homocysteine, an amino acid, can indicate a folate deficiency, as folate is required for its metabolism.
Clinical Evaluation
In addition to laboratory tests, healthcare providers will conduct a thorough clinical evaluation. This may include asking about dietary habits, reviewing any medications the patient is taking, and assessing for underlying medical conditions that could contribute to the deficiency.
Treatment Options for Folate Deficiency
The treatment for folate deficiency primarily focuses on addressing the underlying cause and replenishing folate levels in the body. Depending on the severity of the deficiency and the individual’s specific circumstances, treatment options may include:
Dietary Changes
Increasing dietary intake of folate-rich foods is often the first step in treating a deficiency. Foods that are high in folate include:
- Leafy green vegetables, such as spinach, kale, and collard greens
- Citrus fruits, such as oranges and grapefruits
- Legumes, such as lentils, chickpeas, and beans
- Fortified cereals and grains
- Nuts and seeds
For individuals who struggle to meet their folate needs through diet alone, supplementation may be recommended.
Folate Supplements
Folate supplements are available in various forms, including tablets, capsules, and liquids. The dosage and duration of supplementation will depend on the severity of the deficiency and the individual’s response to treatment. In some cases, healthcare providers may prescribe high-dose folate supplements to quickly correct the deficiency.
Treating Underlying Conditions
If a medical condition or medication is contributing to folate deficiency, addressing these underlying factors is essential for long-term management. For example, individuals with malabsorption disorders may benefit from dietary modifications or medications that improve nutrient absorption. Similarly, adjusting or discontinuing certain medications under medical supervision may help resolve the deficiency.
Lifestyle Modifications
Adopting healthy lifestyle habits can also support folate levels and prevent future deficiencies. These include:
- Limiting alcohol consumption
- Avoiding smoking, as it can deplete folate stores
- Maintaining a balanced and varied diet
Special Considerations for Pregnant Women
Pregnant women have increased folate requirements due to the demands of fetal development. A deficiency during pregnancy can increase the risk of neural tube defects, such as spina bifida, in the developing baby. To mitigate this risk, healthcare providers often recommend folic acid supplements before conception and during early pregnancy. Many countries also mandate the fortification of staple foods, such as bread and cereals, with folic acid to ensure adequate intake among women of childbearing age.
Preventing Folate Deficiency
Prevention is key to avoiding the complications associated with folate deficiency. By adopting a nutrient-rich diet and addressing risk factors early, individuals can maintain optimal folate levels and support overall health. Regular check-ups with a healthcare provider can also help identify and address deficiencies before they become severe.