Pelvic organ prolapse, often abbreviated as POP, is a condition that affects many women worldwide. It occurs when the muscles and tissues supporting the pelvic organs weaken or stretch, causing these organs to drop from their normal positions. One specific type of pelvic organ prolapse is an enterocele, which involves the small intestine pushing into the vaginal wall. This article provides a comprehensive overview of pelvic organ prolapse, including its symptoms, diagnosis, and treatment options.
Understanding Pelvic Organ Prolapse
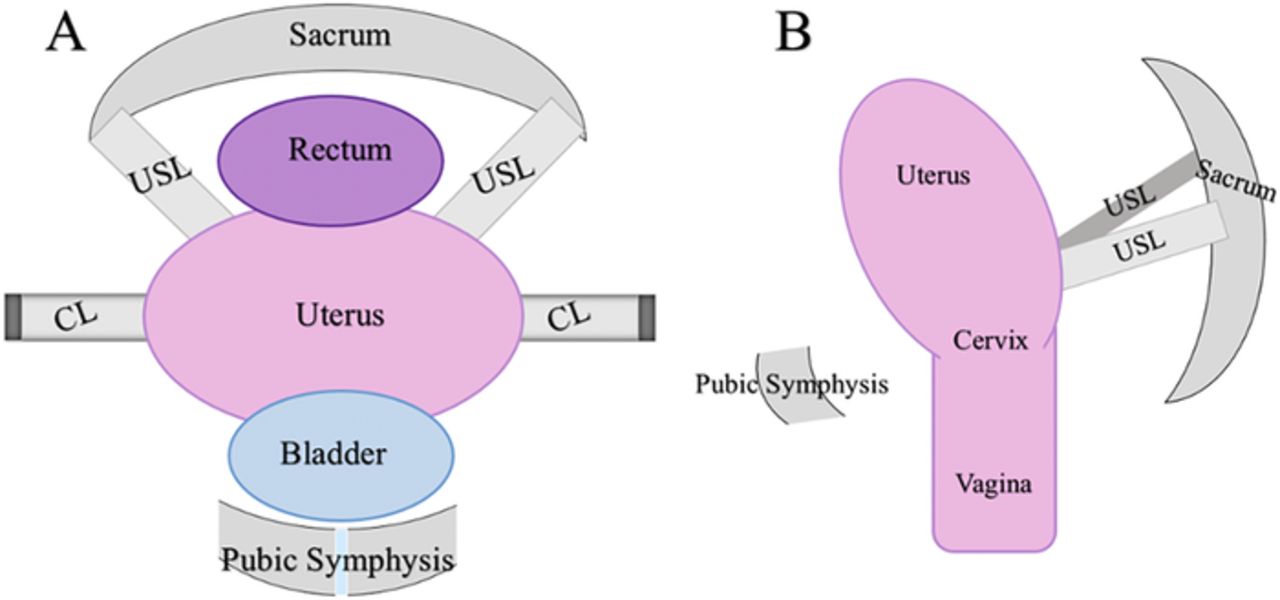
Pelvic organ prolapse is a medical condition where one or more of the pelvic organs descend from their usual position. The pelvic organs include the bladder, uterus, rectum, and small intestine. When the supportive structures in the pelvis become weak or damaged, these organs can shift downward, leading to discomfort and other complications.
Types of Pelvic Organ Prolapse
- Cystocele: Occurs when the bladder bulges into the front wall of the vagina.
- Rectocele: Happens when the rectum pushes into the back wall of the vagina.
- Uterine Prolapse: Involves the uterus descending into or out of the vagina.
- Vaginal Vault Prolapse: Occurs in women who have had a hysterectomy, where the top of the vagina collapses.
- Enterocele: Involves the small intestine protruding into the upper part of the vagina.
Symptoms of Pelvic Organ Prolapse
The symptoms of pelvic organ prolapse can vary depending on the type and severity of the condition. Some women may experience mild symptoms, while others may face significant discomfort. Common symptoms include:
- A sensation of pressure or fullness in the pelvic area.
- A bulge or lump in the vagina.
- Discomfort during sexual intercourse.
- Urinary problems such as incontinence or difficulty emptying the bladder.
- Bowel issues like constipation or incomplete bowel movements.
- Lower back pain.
When to Seek Medical Attention
If you notice any of the above symptoms, it is important to consult a healthcare provider. Early diagnosis and treatment can help manage the condition effectively and prevent further complications.
Diagnosis of Pelvic Organ Prolapse
Diagnosing pelvic organ prolapse involves a thorough evaluation by a healthcare professional. The process typically includes:
Medical History and Physical Examination
Your doctor will begin by taking a detailed medical history to understand your symptoms and any factors that might contribute to the condition. A physical examination will follow, where the healthcare provider will assess the pelvic area for signs of prolapse.
Pelvic Examination
A pelvic examination is crucial for diagnosing pelvic organ prolapse. During this exam, the doctor may ask you to bear down as if having a bowel movement to observe how the pelvic organs respond. This helps identify the type and extent of the prolapse.
Additional Tests
In some cases, additional tests may be necessary to confirm the diagnosis or rule out other conditions. These tests may include:
- Ultrasound: To visualize the pelvic organs and assess their position.
- Magnetic Resonance Imaging (MRI): Provides detailed images of the pelvic structures.
- Urodynamic Testing: Evaluates bladder function and identifies urinary issues related to prolapse.
Treatment Options for Pelvic Organ Prolapse
Treatment for pelvic organ prolapse depends on the severity of the condition, the type of prolapse, and the patient’s overall health and preferences. Options range from lifestyle changes to surgical interventions.
Lifestyle Modifications
For mild cases of pelvic organ prolapse, lifestyle modifications can help alleviate symptoms and prevent the condition from worsening. These include:
- Pelvic Floor Exercises: Strengthening the pelvic floor muscles through exercises like Kegels can provide support to the pelvic organs.
- Weight Management: Maintaining a healthy weight reduces pressure on the pelvic floor.
- Avoiding Heavy Lifting: Reduces strain on the pelvic muscles.
Nonsurgical Treatments
When lifestyle changes are insufficient, nonsurgical treatments may be recommended:
- Pessaries: These are devices inserted into the vagina to support the pelvic organs. They come in various shapes and sizes and can be fitted by a healthcare provider.
- Estrogen Therapy: For postmenopausal women, topical estrogen can help strengthen the vaginal tissues.
Surgical Interventions
In cases where pelvic organ prolapse significantly impacts quality of life, surgery may be necessary. Surgical options include:
- Reconstructive Surgery: Repairs the supportive tissues and restores the normal position of the pelvic organs.
- Hysterectomy: Removal of the uterus may be recommended for uterine prolapse.
- Vaginal Vault Suspension: Used for vaginal vault prolapse, this procedure reattaches the top of the vagina to supportive structures.
- Mesh Implants: Synthetic mesh can be used to provide additional support, though this option carries risks and should be discussed thoroughly with a healthcare provider.
Risks and Considerations
While surgery can effectively treat pelvic organ prolapse, it is not without risks. Potential complications include infection, bleeding, and recurrence of prolapse. It is essential to discuss the benefits and risks with your doctor to make an informed decision.
Living with Pelvic Organ Prolapse
Managing pelvic organ prolapse involves ongoing care and attention. Regular follow-ups with a healthcare provider are important to monitor the condition and adjust treatment as needed. Additionally, adopting healthy habits and staying informed about the condition can empower individuals to take control of their health.
Support and Resources
Living with pelvic organ prolapse can be challenging, but support is available. Many organizations and online communities offer resources and guidance for individuals affected by this condition. Connecting with others who share similar experiences can provide emotional support and practical advice.