Endocarditis, often abbreviated as IE, is a serious medical condition characterized by inflammation of the inner lining of the heart, particularly the heart valves. This condition requires immediate attention due to its potential to cause severe complications if left untreated. In this article, we will explore the causes, symptoms, and care strategies associated with this condition to help you better understand its implications and treatment options.
Understanding Endocarditis
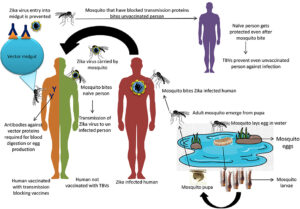
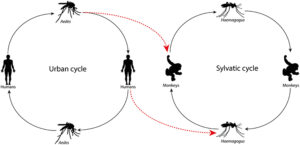
Endocarditis occurs when bacteria, fungi, or other microorganisms enter the bloodstream and attach themselves to damaged areas of the heart. The heart’s inner lining, known as the endocardium, becomes inflamed as a result of this invasion. While the condition can affect anyone, certain individuals are more vulnerable due to pre-existing heart conditions or weakened immune systems.
How Does Endocarditis Develop?
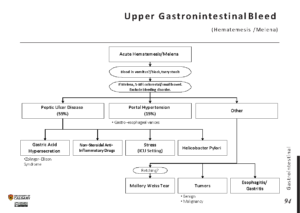
The development of endocarditis typically begins when harmful microorganisms enter the bloodstream. These microorganisms can originate from various sources, such as infections in other parts of the body, dental procedures, or even everyday activities like brushing teeth. Once in the bloodstream, these organisms travel to the heart and settle on the heart valves or other damaged areas of the heart lining. Over time, they multiply and form clusters, leading to inflammation and damage.
Causes of Endocarditis
Several factors can contribute to the development of endocarditis. Understanding these causes is essential for prevention and early detection.
Bacterial Infections
Bacterial infections are the most common cause of endocarditis. Streptococcus and Staphylococcus bacteria are frequently responsible for these infections. These bacteria can enter the bloodstream through:
- Dental procedures that cause bleeding
- Skin infections or wounds
- Urinary tract infections
- Intravenous drug use
Fungal Infections
Although less common, fungal infections can also lead to endocarditis. Individuals with weakened immune systems, such as those undergoing chemotherapy or living with HIV, are at higher risk of developing fungal endocarditis. Fungi like Candida are often implicated in these cases.
Predisposing Factors
Certain medical conditions and lifestyle factors increase the likelihood of developing endocarditis. These include:
- Pre-existing heart conditions, such as congenital heart defects or damaged heart valves
- History of endocarditis
- Implanted medical devices, such as pacemakers or artificial heart valves
- Chronic diseases like diabetes or kidney disease
- Poor dental hygiene
Symptoms of Endocarditis
Recognizing the symptoms of endocarditis is crucial for early diagnosis and treatment. The symptoms can vary depending on the severity of the infection and the individual’s overall health. Some common signs include:
Fever and Chills
A persistent fever and chills are often the first signs of endocarditis. These symptoms may develop gradually or appear suddenly, depending on the underlying cause of the infection.
Fatigue and Weakness
Individuals with endocarditis frequently experience extreme fatigue and weakness. These symptoms can interfere with daily activities and may worsen over time if the condition is not treated.
Heart Murmurs
A new or changing heart murmur is a hallmark symptom of endocarditis. Heart murmurs occur when blood flow through the heart becomes turbulent due to damage or infection of the heart valves.
Joint and Muscle Pain
Many people with endocarditis report unexplained joint and muscle pain. This discomfort can be mistaken for other conditions, such as arthritis, making diagnosis challenging.
Shortness of Breath
As the infection progresses, it can impair the heart’s ability to pump blood effectively. This can lead to shortness of breath, especially during physical activity or while lying down.
Unexplained Weight Loss
Some individuals with endocarditis experience unintentional weight loss due to the body’s response to the infection. This symptom is often accompanied by a loss of appetite.
Skin Changes
Endocarditis can cause visible changes in the skin, such as red or purple spots on the palms of the hands or soles of the feet. Small, painless nodules may also appear on the fingers or toes.
Diagnosis of Endocarditis
Diagnosing endocarditis requires a combination of clinical evaluation, laboratory tests, and imaging studies. Early and accurate diagnosis is critical to prevent complications.
Physical Examination
A healthcare provider will begin by conducting a thorough physical examination. They will listen to the heart for abnormal sounds, such as murmurs, and check for other signs of infection, such as fever or skin changes.
Blood Tests
Blood tests are essential for identifying the presence of bacteria or fungi in the bloodstream. A complete blood count may reveal elevated white blood cell levels, indicating an active infection.
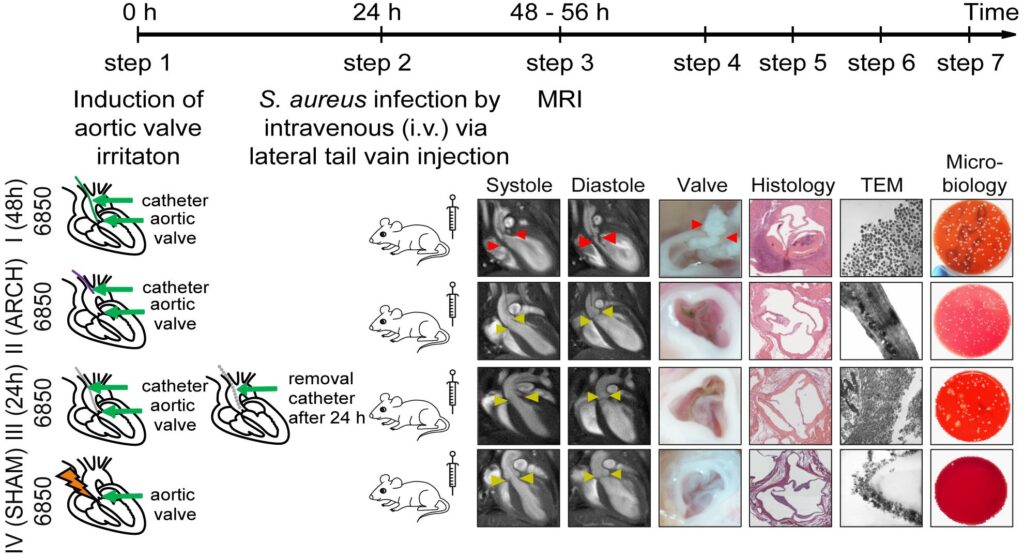
Echocardiography
An echocardiogram uses sound waves to create detailed images of the heart. This test helps identify abnormalities in the heart valves or lining, such as vegetations (clusters of bacteria or fungi).
Other Imaging Studies
In some cases, additional imaging studies, such as a computed tomography scan or magnetic resonance imaging, may be necessary to assess the extent of the infection and its impact on the heart.
Treatment Options for Endocarditis
Treatment for endocarditis typically involves a combination of antibiotics, surgery, and supportive care. The specific approach depends on the severity of the infection and the patient’s overall health.
Antibiotic Therapy
Antibiotics are the primary treatment for bacterial endocarditis. They are usually administered intravenously in a hospital setting to ensure effective delivery to the infected area. The duration of antibiotic therapy can range from several weeks to months, depending on the type of bacteria involved and the patient’s response to treatment.
Surgical Intervention
In severe cases, surgery may be required to repair or replace damaged heart valves. Surgery is also necessary if the infection does not respond to antibiotics or if complications, such as heart failure, arise.
Supportive Care
Supportive care focuses on managing symptoms and preventing complications. This may include medications to reduce fever, pain relievers, and measures to improve heart function.
Prevention Strategies
Preventing endocarditis involves reducing the risk of bacterial infections and maintaining good overall health. Here are some key strategies:
Maintain Good Dental Hygiene
Regular brushing, flossing, and dental check-ups can help prevent infections that could lead to endocarditis. Individuals with pre-existing heart conditions should inform their dentist to ensure appropriate preventive measures are taken during procedures.
Treat Infections Promptly
Addressing infections in other parts of the body, such as skin infections or urinary tract infections, can reduce the risk of bacteria entering the bloodstream.
Practice Safe Intravenous Practices
For individuals who require intravenous therapy or use intravenous drugs, using sterile equipment and techniques is essential to prevent infections.
Follow Medical Advice
Patients with a history of endocarditis or other heart conditions should follow their healthcare provider’s recommendations for preventive antibiotics before certain medical or dental procedures.
Lifestyle Considerations for Managing Endocarditis
In addition to medical treatment, lifestyle adjustments can play a significant role in managing endocarditis and promoting recovery.
Adopt a Heart-Healthy Diet
Eating a balanced diet rich in fruits, vegetables, whole grains, and lean proteins supports overall heart health. Limiting salt, sugar, and unhealthy fats can also reduce the strain on the heart.
Stay Physically Active
Engaging in regular, moderate exercise can improve cardiovascular health and boost the immune system. However, individuals with endocarditis should consult their healthcare provider before starting any exercise program.
Avoid Smoking and Excessive Alcohol Consumption
Smoking and excessive alcohol consumption can weaken the immune system and exacerbate heart conditions. Quitting smoking and moderating alcohol intake are important steps for long-term health.
Manage Stress
Chronic stress can negatively impact heart health. Techniques such as meditation, yoga, and deep breathing exercises can help manage stress and promote relaxation.
Complications Associated with Endocarditis
If left untreated, endocarditis can lead to serious complications that affect multiple organs and systems in the body. Some potential complications include:
Heart Failure
Damage to the heart valves can impair the heart’s ability to pump blood effectively, leading to heart failure.
Stroke
Clumps of bacteria or fungi can break loose from the heart and travel to the brain, causing a stroke.
Kidney Damage
The immune system’s response to the infection can cause inflammation in the kidneys, leading to reduced kidney function.
Spread of Infection
The infection can spread to other parts of the body, such as the lungs, spleen, or bones, causing additional complications.