Pregnancy is a transformative period in a woman’s life, but it can also bring challenges that require careful attention. One such challenge is eclampsia, a serious and potentially life-threatening condition that affects pregnant women. Often abbreviated as “E,” this complication is a progression of preeclampsia, another dangerous pregnancy-related disorder. In this article, we will delve into what eclampsia is, its causes, symptoms, risk factors, diagnosis, treatment options, and prevention strategies.
What is Eclampsia?
Eclampsia is a severe condition that occurs during pregnancy or shortly after childbirth. It is characterized by the onset of seizures or convulsions in a pregnant woman who has already been diagnosed with preeclampsia. Preeclampsia itself is marked by high blood pressure and signs of damage to other organ systems, most commonly the liver and kidneys. When left untreated, preeclampsia can escalate into eclampsia, which poses significant risks to both the mother and the unborn child.
The exact cause of eclampsia remains unclear, but researchers believe it involves abnormalities in the placenta, immune system dysfunction, and genetic predispositions. The condition typically develops after the 20th week of pregnancy, although it can occur earlier or even postpartum.
Symptoms of Eclampsia
Recognizing the symptoms of eclampsia is critical for timely intervention. Some common signs include:
- Sudden and severe headaches
- Blurred vision or temporary loss of vision
- Upper abdominal pain, often under the ribs on the right side
- Nausea and vomiting
- Swelling in the hands, face, or legs
- Decreased urine output
- Seizures or convulsions
It is important to note that some women may not exhibit noticeable symptoms until the condition has progressed significantly. Regular prenatal care plays a vital role in early detection and management.
Causes and Risk Factors
While the precise cause of eclampsia remains unknown, several contributing factors have been identified. These include:
Placental Issues
The placenta, which nourishes the developing fetus, plays a central role in the development of eclampsia. Abnormalities in the way the placenta attaches to the uterine wall can lead to restricted blood flow. This restriction can trigger a cascade of events, including high blood pressure and organ damage, which are hallmarks of preeclampsia and eclampsia.
Immune System Dysfunction
Some studies suggest that an overactive immune response may contribute to the development of eclampsia. During pregnancy, the mother’s immune system must adapt to accommodate the presence of the fetus, which contains genetic material from both parents. If this adaptation fails, it can result in inflammation and vascular complications.
Genetic Predisposition
Women with a family history of preeclampsia or eclampsia are at a higher risk of developing the condition themselves. Genetic factors may influence how the body responds to pregnancy-related changes, making some women more susceptible than others.
Other Risk Factors
In addition to the above causes, certain factors increase the likelihood of developing eclampsia:
- First-time pregnancies
- History of chronic hypertension or kidney disease
- Being pregnant with multiple babies (twins, triplets, etc.)
- Maternal age younger than 20 or older than 40
- Obesity
- Diabetes
- Autoimmune disorders such as lupus
Diagnosis of Eclampsia
Diagnosing eclampsia involves a combination of clinical evaluation, laboratory tests, and monitoring. Healthcare providers rely on the following methods to confirm the condition:
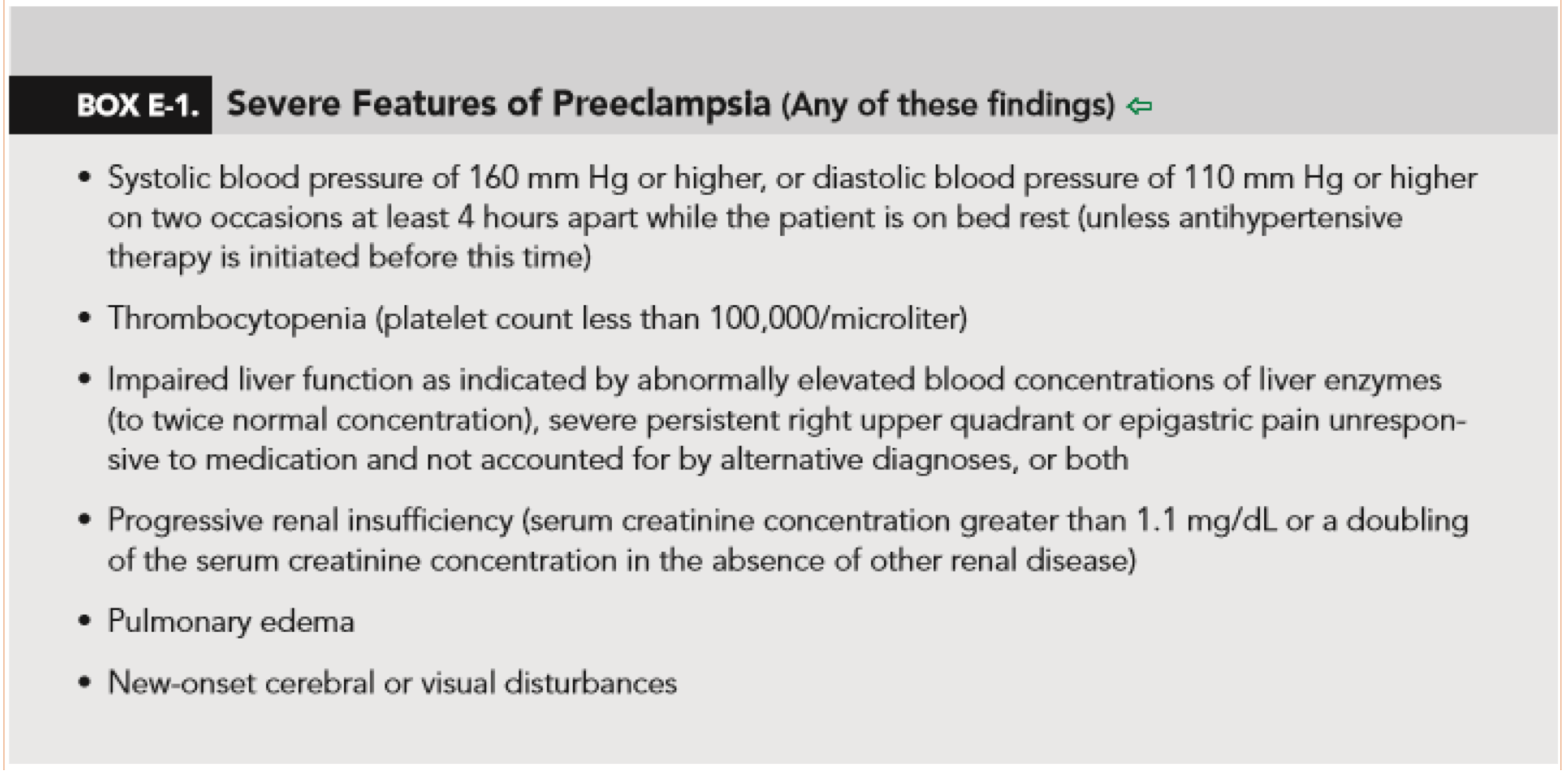
Blood Pressure Monitoring
High blood pressure is one of the primary indicators of preeclampsia, which can progress to eclampsia. Blood pressure readings consistently above 140/90 mmHg are considered abnormal during pregnancy and warrant further investigation.
Urine Tests
Proteinuria, or the presence of excess protein in the urine, is another key sign of preeclampsia. A urine test can help determine whether protein levels are elevated, indicating potential kidney damage.
Blood Tests
Blood tests are used to assess liver and kidney function, as well as platelet counts. Abnormal results in these areas may suggest organ damage associated with eclampsia.
Fetal Monitoring
Monitoring the health of the fetus is crucial when diagnosing eclampsia. Ultrasound scans and non-stress tests can provide insights into fetal growth and well-being, helping healthcare providers make informed decisions about treatment.
Treatment Options for Eclampsia
Once eclampsia is diagnosed, immediate medical intervention is necessary to protect the lives of both the mother and the baby. Treatment focuses on managing symptoms, preventing seizures, and delivering the baby as safely as possible.
Medications
Several medications are commonly used to treat eclampsia:
- Anticonvulsants: Medications such as magnesium sulfate are administered to prevent or control seizures. Magnesium sulfate is highly effective in reducing the risk of eclamptic seizures and is considered the first-line treatment.
- Antihypertensives: Drugs that lower blood pressure may be prescribed to manage severe hypertension. However, these medications must be carefully monitored to avoid reducing blood flow to the placenta.
Delivery of the Baby
In many cases, the only definitive treatment for eclampsia is the delivery of the baby. If the pregnancy has reached a viable stage (typically after 34 weeks), inducing labor or performing a cesarean section may be recommended. Early delivery may also be necessary if the mother’s or baby’s health is at significant risk.
Hospitalization and Monitoring
Women diagnosed with eclampsia often require hospitalization for close monitoring. This allows healthcare providers to manage symptoms effectively and respond quickly to any complications that arise.
Prevention Strategies
While eclampsia cannot always be prevented, certain measures can reduce the risk of its development:
Regular Prenatal Care
Attending all scheduled prenatal appointments is essential for early detection of preeclampsia and other complications. Routine check-ups allow healthcare providers to monitor blood pressure, urine protein levels, and overall maternal health.
Healthy Lifestyle Choices
Maintaining a healthy lifestyle before and during pregnancy can lower the risk of eclampsia. Key recommendations include:
- Eating a balanced diet rich in fruits, vegetables, whole grains, and lean proteins
- Exercising regularly, as advised by a healthcare provider
- Avoiding smoking, alcohol, and recreational drugs
- Managing pre-existing conditions such as diabetes and hypertension
Low-Dose Aspirin
For women at high risk of developing preeclampsia, low-dose aspirin may be prescribed starting in the first trimester. Studies have shown that this medication can reduce the risk of preeclampsia and, by extension, eclampsia.
Calcium Supplementation
In regions where dietary calcium intake is low, calcium supplements may help prevent preeclampsia. Women should consult their healthcare provider before starting any supplementation regimen.
Living with Eclampsia: Emotional and Physical Challenges
Eclampsia not only affects physical health but also takes an emotional toll on expectant mothers and their families. The uncertainty and severity of the condition can lead to anxiety, stress, and feelings of helplessness. Support from loved ones, healthcare providers, and mental health professionals can play a crucial role in helping women cope with these challenges.
Postpartum Recovery
Even after delivery, women who have experienced eclampsia may require ongoing medical care. Blood pressure levels often remain elevated for several weeks postpartum, necessitating continued monitoring and treatment. Additionally, women who have had eclampsia are at increased risk for cardiovascular diseases later in life, underscoring the importance of long-term health management.
Impact on Future Pregnancies
Women who have had eclampsia in one pregnancy are at a higher risk of experiencing it again in subsequent pregnancies. Close monitoring and proactive management are essential to ensure safe outcomes in future pregnancies.