Persistent Depressive Disorder, often abbreviated as PDD, is a chronic form of depression that affects millions of people worldwide. Unlike major depressive episodes that may come and go, this condition lingers for years, subtly but persistently impacting an individual’s quality of life. Understanding the nuances of this mental health condition is crucial for both those who experience it and their loved ones. In this article, we will explore Persistent Depressive Disorder in detail, covering its symptoms, causes, diagnosis, treatment options, and coping strategies.
What Is Persistent Depressive Disorder?
Persistent Depressive Disorder is a long-term form of depression characterized by a consistently low mood that lasts for at least two years in adults and one year in children or adolescents. While the symptoms may not be as severe as those of major depressive disorder, they are persistent enough to interfere with daily functioning and overall well-being. People with this condition often describe feeling “down” or “gloomy” most of the time, even during moments of joy or success.
Key Features of Persistent Depressive Disorder
- A pervasive sense of sadness or emptiness
- Fatigue or lack of energy
- Difficulty concentrating or making decisions
- Feelings of hopelessness or worthlessness
- Changes in appetite or weight
- Sleep disturbances, such as insomnia or oversleeping
- Low self-esteem
These symptoms can vary in intensity but tend to remain present over extended periods. For some individuals, there may be periods of relative relief, but the core symptoms typically return without proper intervention.
Causes and Risk Factors
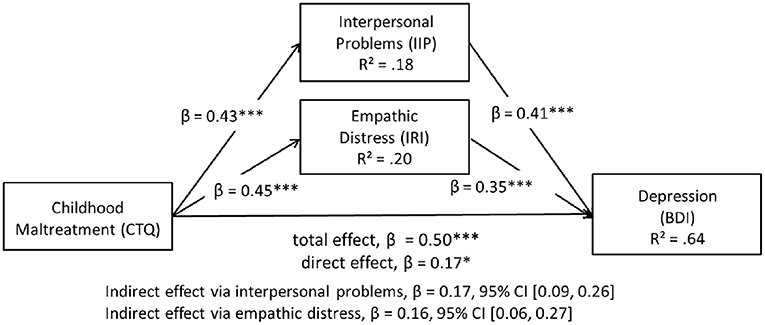
The exact cause of Persistent Depressive Disorder remains unclear, but research suggests that it arises from a combination of biological, psychological, and environmental factors. Understanding these influences can help shed light on why some individuals develop this condition while others do not.
Biological Factors
Several biological mechanisms may contribute to the development of Persistent Depressive Disorder:
- Genetics: Individuals with a family history of depression or other mood disorders are at a higher risk of developing this condition.
- Brain Chemistry: Imbalances in neurotransmitters, such as serotonin and dopamine, which regulate mood, may play a role in the onset of depressive symptoms.
- Hormonal Changes: Fluctuations in hormone levels, particularly during puberty, pregnancy, or menopause, can increase vulnerability to depression.
Psychological Factors
Personality traits and cognitive patterns can also influence the likelihood of developing Persistent Depressive Disorder:
- Negative Thinking Patterns: Chronic pessimism or a tendency to focus on negative experiences can perpetuate feelings of sadness and hopelessness.
- Low Self-Esteem: Individuals who struggle with feelings of inadequacy or self-worth may be more prone to depressive symptoms.
- Trauma or Stress: Experiencing significant life stressors, such as abuse, loss, or financial difficulties, can trigger or exacerbate depressive episodes.
Environmental Factors
External circumstances can significantly impact mental health and contribute to the development of Persistent Depressive Disorder:
- Social Isolation: Lack of social support or meaningful relationships can worsen feelings of loneliness and despair.
- Chronic Illness: Living with a long-term medical condition can lead to emotional distress and depressive symptoms.
- Substance Abuse: Alcohol or drug misuse can both contribute to and result from depressive disorders.
Diagnosing Persistent Depressive Disorder
Diagnosing Persistent Depressive Disorder involves a comprehensive evaluation by a mental health professional. Since the symptoms can overlap with other conditions, such as major depressive disorder or anxiety disorders, accurate diagnosis is essential for effective treatment.
Diagnostic Criteria
To meet the criteria for Persistent Depressive Disorder, an individual must exhibit a depressed mood for most of the day, nearly every day, for at least two years (or one year for children and adolescents). During this period, they must also experience at least two of the following symptoms:
- Poor appetite or overeating
- Insomnia or hypersomnia
- Low energy or fatigue
- Low self-esteem
- Poor concentration or difficulty making decisions
- Feelings of hopelessness
Assessment Process
Mental health professionals typically use interviews, questionnaires, and standardized assessment tools to gather information about an individual’s symptoms, medical history, and life circumstances. They may also conduct physical exams or order laboratory tests to rule out underlying medical conditions that could mimic depressive symptoms.
Treatment Options for Persistent Depressive Disorder
While Persistent Depressive Disorder is a chronic condition, it is highly treatable with the right interventions. Treatment often involves a combination of psychotherapy, medication, and lifestyle changes tailored to the individual’s needs.
Psychotherapy
Psychotherapy, or talk therapy, is a cornerstone of treatment for Persistent Depressive Disorder. It provides individuals with tools to manage their symptoms, challenge negative thought patterns, and improve their emotional resilience. Some common therapeutic approaches include:
- Cognitive Behavioral Therapy (CBT): Focuses on identifying and changing unhelpful thoughts and behaviors that contribute to depression.
- Interpersonal Therapy (IPT): Addresses relationship issues and improves communication skills to reduce interpersonal stress.
- Psychodynamic Therapy: Explores unconscious processes and unresolved conflicts that may underlie depressive symptoms.
Medication
Antidepressant medications can be effective in alleviating symptoms of Persistent Depressive Disorder. The most commonly prescribed classes of antidepressants include:
- Selective Serotonin Reuptake Inhibitors (SSRIs): Increase serotonin levels in the brain to improve mood.
- Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs): Target both serotonin and norepinephrine to enhance emotional regulation.
- Tricyclic Antidepressants (TCAs): An older class of medications that may be used when other treatments are ineffective.
It is important to note that finding the right medication and dosage may take time, and side effects should be closely monitored by a healthcare provider.
Lifestyle Changes
In addition to professional treatment, certain lifestyle modifications can complement therapy and medication. These changes can help individuals better manage their symptoms and improve their overall well-being:
- Regular Exercise: Physical activity has been shown to boost mood and reduce symptoms of depression.
- Healthy Diet: Consuming nutrient-rich foods can support brain health and stabilize mood.
- Sleep Hygiene: Establishing a consistent sleep routine can alleviate fatigue and improve concentration.
- Mindfulness Practices: Techniques such as meditation and yoga can promote relaxation and emotional balance.
Coping Strategies for Individuals and Families
Living with Persistent Depressive Disorder can be challenging, but adopting effective coping strategies can make a significant difference. Both individuals with the condition and their loved ones can benefit from practical approaches to managing its impact.
For Individuals
Here are some strategies that individuals can use to cope with Persistent Depressive Disorder:
- Set Realistic Goals: Break tasks into smaller, manageable steps to avoid feeling overwhelmed.
- Practice Self-Compassion: Be kind to yourself and recognize that recovery is a gradual process.
- Stay Connected: Reach out to friends, family, or support groups to combat feelings of isolation.
- Monitor Symptoms: Keep a journal to track mood changes and identify potential triggers.
For Families and Caregivers
Families and caregivers play a vital role in supporting individuals with Persistent Depressive Disorder. Here are some ways they can help:
- Educate Yourself: Learn about the condition to better understand what your loved one is experiencing.
- Offer Emotional Support: Listen without judgment and validate their feelings.
- Encourage Professional Help: Gently suggest seeking therapy or consulting a doctor if needed.
- Take Care of Yourself: Prioritize your own mental and physical health to avoid burnout.
Addressing Stigma and Misconceptions
Despite growing awareness of mental health issues, stigma surrounding depression persists. Many individuals with Persistent Depressive Disorder may hesitate to seek help due to fear of judgment or misunderstanding. Addressing these misconceptions is essential for fostering a supportive environment where people feel comfortable discussing their struggles.
One common misconception is that depression is simply a matter of “snapping out of it” or having a negative attitude. In reality, Persistent Depressive Disorder is a legitimate medical condition rooted in complex biological and psychological factors. Educating the public about the nature of this disorder can help reduce stigma and encourage more people to seek treatment.
Final Thoughts
Persistent Depressive Disorder is a challenging yet manageable condition that requires patience, persistence, and a multifaceted approach to treatment. By understanding its symptoms, causes, and available interventions, individuals and their loved ones can take proactive steps toward healing and improved quality of life.