Dysentery, a term often abbreviated as “DY,” is a significant health concern worldwide. It refers to an inflammatory condition of the intestines, particularly the colon, that leads to severe diarrhea with blood or mucus in the stool. This condition affects millions of people annually, especially in regions with poor sanitation and limited access to clean water. Understanding dysentery, including its causes, symptoms, types, and treatments, is essential for preventing its spread and managing its effects on individuals and communities.
What Causes Dysentery?
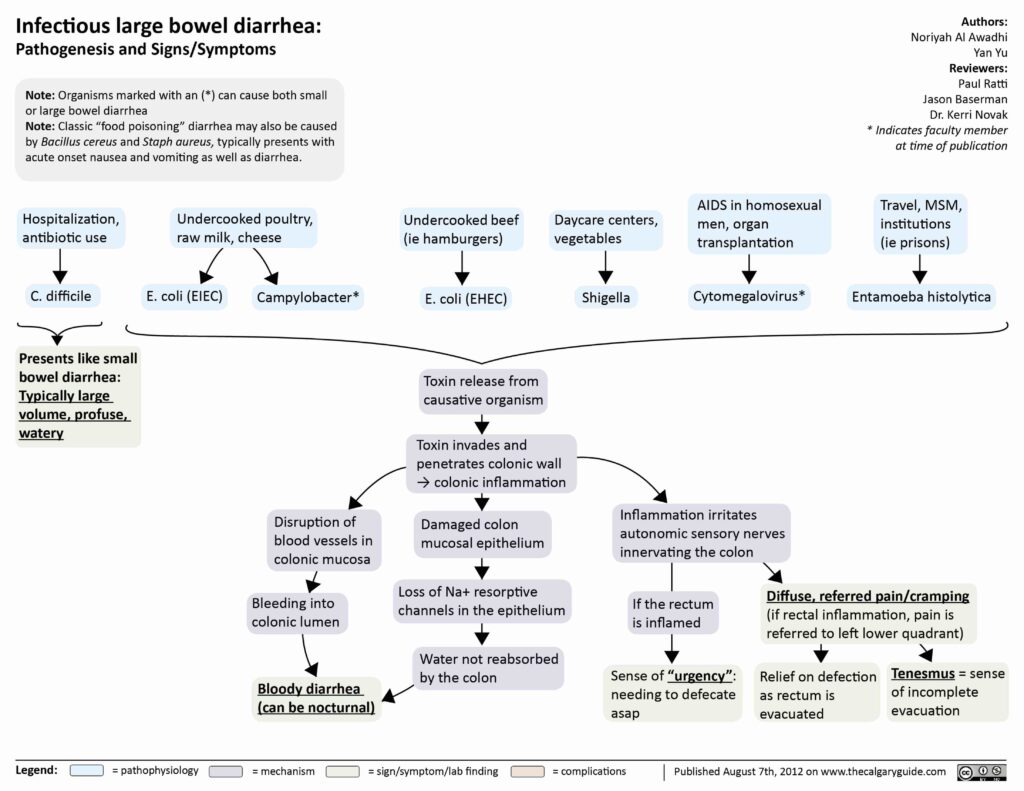
Dysentery is primarily caused by infections resulting from bacteria, viruses, or parasites. The most common sources of infection include contaminated food, water, and poor hygiene practices. Below are the primary causes of dysentery:
Bacterial Infections
- Shigella Bacteria: Shigella species are responsible for a type of dysentery known as bacillary dysentery. These bacteria invade the lining of the intestines, causing inflammation and damage to the intestinal walls.
- Escherichia coli: Certain strains of Escherichia coli can also lead to dysentery, particularly enterohemorrhagic E. coli, which produces toxins that harm the intestines.
Parasitic Infections
- Entamoeba histolytica: This parasite is responsible for amoebic dysentery. It invades the intestinal lining and can spread to other organs, such as the liver, causing abscesses.
Viral Infections
- Norovirus and Rotavirus: While less common, viral infections can sometimes result in dysentery-like symptoms, particularly in children and individuals with weakened immune systems.
Other Contributing Factors
- Poor sanitation and lack of clean drinking water increase the risk of exposure to pathogens that cause dysentery.
- Crowded living conditions, such as refugee camps or areas affected by natural disasters, facilitate the rapid spread of the disease.
- Consumption of raw or undercooked food, especially meat and seafood, can introduce harmful bacteria or parasites into the body.
Symptoms of Dysentery
The symptoms of dysentery can vary depending on the causative agent and the severity of the infection. However, some common signs and symptoms are observed across most cases:
Gastrointestinal Symptoms
- Frequent passage of loose stools, often containing blood or mucus.
- Abdominal pain and cramping, which may be severe in some cases.
- Tenesmus, or the constant urge to pass stools despite having an empty bowel.
Systemic Symptoms
- Fever, which may range from mild to high-grade depending on the severity of the infection.
- Dehydration caused by excessive fluid loss through diarrhea and vomiting.
- Fatigue and weakness due to the body’s response to infection and dehydration.
Severe Symptoms
- In extreme cases, dysentery can lead to complications such as sepsis, perforation of the intestinal wall, or toxic megacolon.
- Individuals with amoebic dysentery may experience liver abscesses if the infection spreads beyond the intestines.
Types of Dysentery
Dysentery is broadly categorized into two main types based on the causative agents: bacillary dysentery and amoebic dysentery. Each type has distinct characteristics and requires specific treatment approaches.
Bacillary Dysentery
Bacillary dysentery is caused by bacteria, primarily species of Shigella. This form of dysentery is highly contagious and spreads rapidly in environments with poor hygiene. Key features of bacillary dysentery include:
- Sudden onset of symptoms within one to three days after exposure to the bacteria.
- Presence of blood and mucus in stools, accompanied by abdominal pain and fever.
- Self-limiting nature in mild cases, but severe cases may require medical intervention to prevent complications.
Amoebic Dysentery
Amoebic dysentery is caused by the parasite Entamoeba histolytica. Unlike bacillary dysentery, this type can have a more insidious onset and may persist for weeks or months if untreated. Characteristics of amoebic dysentery include:
- Gradual development of symptoms, with intermittent episodes of diarrhea and constipation.
- Stools that contain blood and mucus, along with significant abdominal discomfort.
- Potential for systemic complications, such as liver abscesses, if the parasite spreads beyond the intestines.
Treatments for Dysentery
The treatment of dysentery depends on the underlying cause, the severity of symptoms, and the overall health of the individual. Prompt diagnosis and appropriate management are crucial to prevent complications and ensure recovery.
Rehydration Therapy
One of the primary goals of treating dysentery is to address dehydration caused by fluid loss. Rehydration therapy is essential and can be administered in the following ways:
- Oral Rehydration Solutions: These solutions contain a balanced mix of salts and sugars to replenish lost fluids and electrolytes. They are effective for mild to moderate dehydration.
- Intravenous Fluids: In cases of severe dehydration, intravenous fluids may be necessary to restore hydration quickly.
Antibiotics
For bacterial dysentery, antibiotics are often prescribed to eliminate the infection. Commonly used antibiotics include:
- Ciprofloxacin and azithromycin for treating Shigella infections.
- Metronidazole or tinidazole for amoebic dysentery caused by Entamoeba histolytica.
It is important to note that antibiotic resistance is a growing concern, and misuse of antibiotics can worsen the problem. Therefore, these medications should only be taken under medical supervision.
Antiparasitic Medications
In cases of amoebic dysentery, antiparasitic drugs are essential to eradicate the parasite. Metronidazole is typically used as the first-line treatment, followed by a luminal agent like paromomycin to eliminate any remaining cysts in the intestines.
Symptomatic Treatment
In addition to addressing the root cause of dysentery, symptomatic treatment can help alleviate discomfort and improve quality of life during recovery. This includes:
- Over-the-counter medications to reduce fever and relieve pain, such as acetaminophen or ibuprofen.
- Avoidance of anti-diarrheal medications like loperamide, as they can prolong the infection by slowing down the elimination of pathogens from the body.
Dietary Adjustments
During recovery, dietary modifications can support healing and prevent further irritation of the digestive system. Recommendations include:
- Consuming bland, easily digestible foods such as rice, bananas, applesauce, and toast.
- Avoiding spicy, fatty, or high-fiber foods that may exacerbate symptoms.
- Ensuring adequate intake of fluids to maintain hydration.
Preventive Measures
Preventing dysentery involves adopting practices that reduce exposure to pathogens. Key preventive measures include:
- Access to clean drinking water and proper sanitation facilities.
- Regular handwashing with soap and water, especially before eating and after using the toilet.
- Proper cooking and storage of food to prevent contamination.
- Vaccination against rotavirus, which can help reduce the incidence of viral gastroenteritis in children.