Shoulder dislocation, often abbreviated as SD, is a common musculoskeletal injury that occurs when the upper arm bone is forced out of its normal position in the shoulder socket. This condition can be painful and debilitating, affecting daily activities and requiring prompt medical attention. In this article, we will explore the causes, symptoms, diagnosis, and treatment options for shoulder dislocation to provide a comprehensive understanding of this injury.
What Is Shoulder Dislocation?
The shoulder is one of the most mobile joints in the human body, allowing for a wide range of motion. However, this mobility comes at the cost of stability, making the shoulder joint more prone to dislocations. A shoulder dislocation happens when the head of the humerus (upper arm bone) slips out of the glenoid cavity, which is part of the shoulder blade. This can occur in different directions, with anterior dislocations being the most common.
Types of Shoulder Dislocations
- Anterior Dislocation: The head of the humerus moves forward out of the socket. This accounts for about 95 percent of all shoulder dislocations.
- Posterior Dislocation: The head of the humerus moves backward out of the socket. This type is less common and often associated with specific injuries or medical conditions.
- Inferior Dislocation: The head of the humerus moves downward out of the socket. This is the rarest form of shoulder dislocation.
Causes of Shoulder Dislocation
Shoulder dislocations are typically caused by trauma or repetitive strain on the joint. Below are some common causes of this injury:
Traumatic Events
Trauma is the leading cause of shoulder dislocations. High-impact events such as falls, sports injuries, or motor vehicle accidents can force the shoulder out of its socket. Contact sports like football, rugby, and wrestling pose a higher risk due to the physical nature of these activities.
Falls
Falling onto an outstretched hand or directly onto the shoulder can lead to dislocation. This is especially common among older adults who may have weaker bones or reduced muscle strength to stabilize the joint.
Repetitive Strain
Activities that involve repetitive overhead motions, such as swimming, tennis, or weightlifting, can weaken the ligaments around the shoulder joint over time. This increases the likelihood of dislocation, particularly in individuals who do not engage in proper warm-ups or conditioning exercises.
Underlying Medical Conditions
Certain medical conditions can predispose individuals to shoulder dislocations. For example, people with hypermobility syndromes, such as Ehlers-Danlos syndrome, or those with previous shoulder injuries may have looser ligaments, making their shoulders more susceptible to dislocation.
Symptoms of Shoulder Dislocation
Recognizing the symptoms of a shoulder dislocation is crucial for seeking timely medical care. The following signs are commonly associated with this injury:
Pain
Intense pain is usually the first symptom experienced after a shoulder dislocation. The pain may radiate down the arm and worsen with movement or touch.
Visible Deformity
In many cases, the shoulder may appear misshapen or out of place. This is especially noticeable in anterior dislocations, where the head of the humerus protrudes forward.
Swelling and Bruising
Swelling and bruising around the shoulder area are common after a dislocation. These symptoms result from soft tissue damage and bleeding within the joint.
Limited Mobility
A dislocated shoulder often results in a significant loss of movement. Individuals may find it difficult or impossible to move their arm without experiencing severe pain.
Numbness or Tingling
In some cases, nerve damage may occur during a shoulder dislocation, leading to numbness or tingling sensations in the arm or fingers. This requires immediate medical evaluation to prevent long-term complications.
Diagnosis of Shoulder Dislocation
Accurate diagnosis is essential for determining the appropriate treatment plan. Healthcare providers use a combination of physical examinations and imaging tests to confirm a shoulder dislocation.
Physical Examination
During a physical examination, the doctor will assess the appearance and alignment of the shoulder. They may gently palpate the area to check for tenderness, swelling, or deformities. Additionally, they will evaluate the patient’s range of motion and ability to perform basic movements.
Imaging Tests
To confirm the diagnosis and rule out additional injuries, imaging tests are often required:
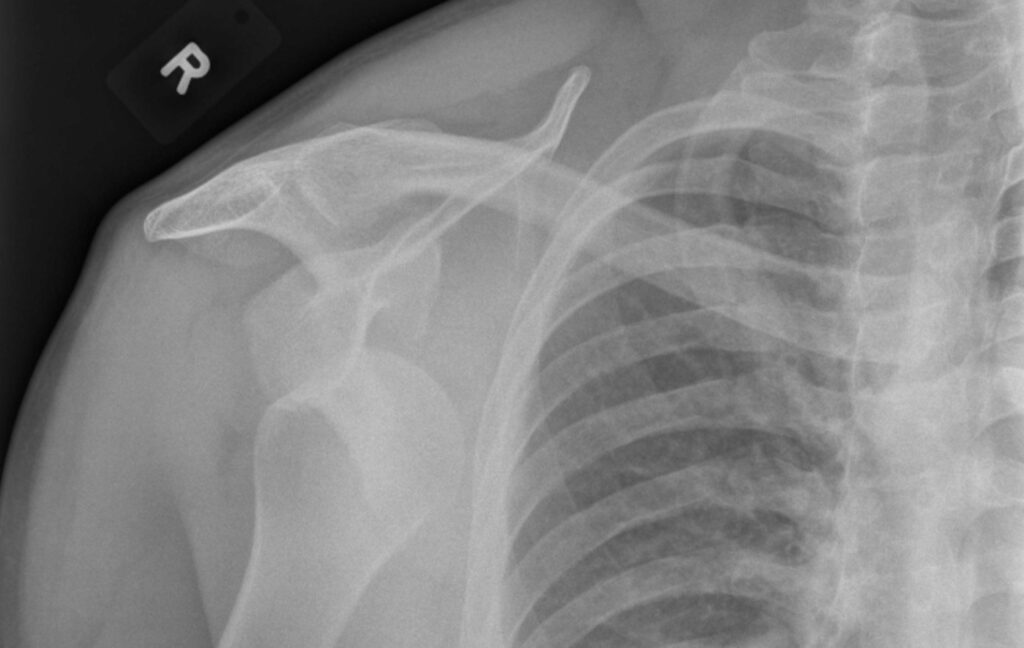
- X-rays: X-ray images help identify the position of the dislocated bone and detect fractures or other structural abnormalities.
- Magnetic Resonance Imaging (MRI): An MRI provides detailed images of soft tissues, including ligaments, tendons, and cartilage, to assess the extent of damage.
- Computed Tomography (CT) Scan: A CT scan may be used to obtain a three-dimensional view of the shoulder joint, particularly in complex cases.
Treatment Options for Shoulder Dislocation
The treatment for a shoulder dislocation depends on the severity of the injury and whether there are any associated complications. The primary goal is to realign the joint and restore function while minimizing the risk of recurrence.
Immediate Care
Before seeking professional medical help, it is important to immobilize the injured shoulder to prevent further damage. Applying ice packs to reduce swelling and taking over-the-counter pain relievers can also provide temporary relief.
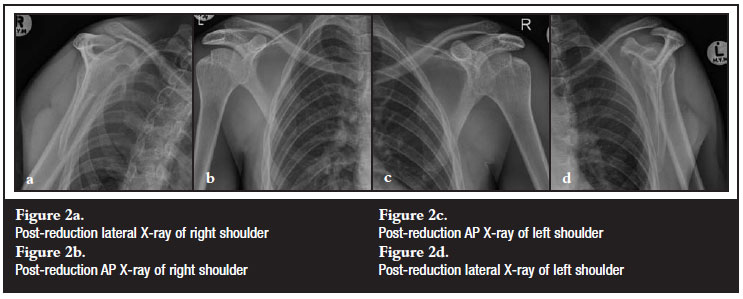
Reduction
Reduction refers to the process of manually repositioning the dislocated bone back into its socket. This procedure should only be performed by trained healthcare professionals to avoid causing additional harm. Various techniques, such as traction-countertraction or scapular manipulation, may be employed depending on the type of dislocation.
Immobilization
After reduction, the shoulder is typically immobilized using a sling or brace to allow the surrounding tissues to heal. The duration of immobilization varies based on the severity of the injury but generally lasts between one and three weeks.
Physical Therapy
Once the initial healing phase is complete, physical therapy plays a critical role in restoring strength, flexibility, and range of motion. A tailored rehabilitation program may include exercises to strengthen the rotator cuff muscles and improve joint stability.
Surgical Intervention
In cases of recurrent dislocations or severe soft tissue damage, surgery may be necessary. Common surgical procedures include:
- Arthroscopy: Minimally invasive surgery to repair torn ligaments or remove damaged tissue.
- Open Surgery: Used for more extensive repairs, such as reconstructing the shoulder capsule or stabilizing the joint.
Pain Management
Pain management strategies are integral to the recovery process. Alongside medications, non-pharmacological approaches such as acupuncture, massage therapy, or transcutaneous electrical nerve stimulation (TENS) may be recommended to alleviate discomfort.
Preventing Shoulder Dislocations
While not all shoulder dislocations can be prevented, certain measures can reduce the risk of injury:
- Engage in regular strength training and flexibility exercises to maintain joint stability.
- Use proper techniques and protective gear during sports or physical activities.
- Avoid overexertion and take breaks to rest the shoulder during repetitive tasks.
- Seek early treatment for minor shoulder injuries to prevent them from worsening.
Living With a Dislocated Shoulder
Recovering from a shoulder dislocation can be challenging, both physically and emotionally. It is important to follow the prescribed treatment plan and communicate openly with healthcare providers about any concerns or setbacks. Support from family, friends, and support groups can also aid in the healing journey.