Dilated Cardiomyopathy, often abbreviated as DCM, is a condition that affects the heart’s ability to pump blood effectively. This occurs when the heart muscle becomes weakened and stretched, leading to an enlarged heart. If left untreated, it can result in serious complications such as heart failure, irregular heartbeats, or even sudden cardiac arrest. Understanding this condition, its symptoms, diagnosis methods, and care options is essential for managing it effectively.
What is Dilated Cardiomyopathy?
Dilated Cardiomyopathy is a type of heart disease characterized by the enlargement and weakening of the heart’s main pumping chamber, known as the left ventricle. As the heart stretches and weakens, it struggles to pump blood efficiently throughout the body. Over time, this leads to reduced oxygen and nutrient delivery to vital organs, causing fatigue, shortness of breath, and other symptoms.
This condition can affect people of all ages but is more commonly diagnosed in adults between the ages of 20 and 60. It may develop due to genetic factors, underlying health conditions, or lifestyle choices. In some cases, the exact cause remains unknown, making it challenging to predict or prevent.
Common Causes of Dilated Cardiomyopathy
- Genetic Factors: A family history of heart conditions can increase the risk of developing this disease.
- Coronary Artery Disease: Blockages in the arteries supplying blood to the heart can weaken the heart muscle over time.
- Infections: Viral infections, such as myocarditis, can damage the heart muscle and lead to enlargement.
- High Blood Pressure: Prolonged hypertension forces the heart to work harder, eventually causing it to enlarge.
- Substance Abuse: Excessive alcohol consumption or drug use can harm the heart muscle.
- Pregnancy: In rare cases, pregnancy-related stress can trigger heart enlargement, a condition known as peripartum cardiomyopathy.
Symptoms of Dilated Cardiomyopathy
The symptoms of this condition can vary depending on the severity of the disease and how much the heart has been affected. Some individuals may experience mild symptoms, while others may face severe complications. Early detection is crucial for effective management.
Early Warning Signs
- Fatigue: Feeling unusually tired or weak, even after minimal physical activity.
- Shortness of Breath: Difficulty breathing during exercise or while lying down.
- Swelling: Fluid retention in the legs, ankles, feet, or abdomen.
- Rapid Heartbeat: A sensation of fluttering or pounding in the chest.
- Chest Pain: Discomfort or pressure in the chest, especially during physical exertion.
Advanced Symptoms
As the condition progresses, more severe symptoms may appear. These include:
- Fainting: Sudden loss of consciousness due to insufficient blood flow to the brain.
- Irregular Heartbeats: Palpitations or arrhythmias that disrupt normal heart function.
- Difficulty Concentrating: Reduced blood flow to the brain can impair cognitive abilities.
- Weight Gain: Rapid weight gain caused by fluid retention.
Diagnosing Dilated Cardiomyopathy
Diagnosing this condition involves a combination of medical evaluations, imaging tests, and laboratory analyses. Early diagnosis allows for timely intervention and better outcomes.
Initial Assessment
A healthcare provider will begin by reviewing the patient’s medical history and conducting a physical examination. They may ask about symptoms, family history of heart disease, and lifestyle habits. Listening to the heart and lungs with a stethoscope can reveal abnormal sounds, such as murmurs or crackles, which may indicate heart problems.
Diagnostic Tests
To confirm the presence of this condition, doctors may order several tests:
- Echocardiogram: This ultrasound test provides detailed images of the heart’s structure and function. It helps measure the size of the heart chambers and assess how well the heart is pumping.
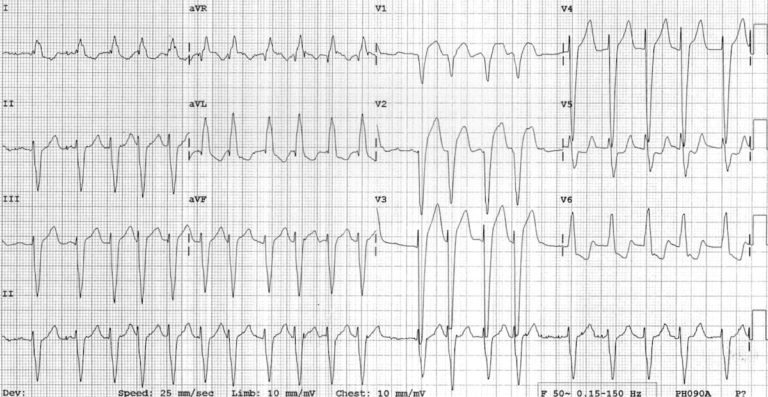
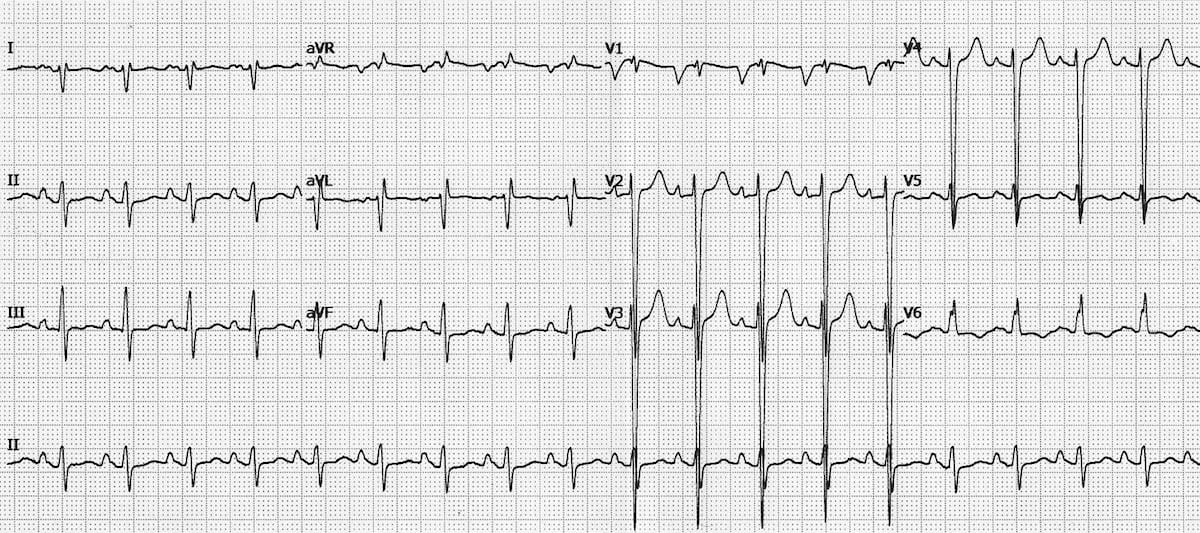
- Electrocardiogram: Also known as an ECG, this test records the electrical activity of the heart. It can detect irregular heart rhythms or signs of heart damage.
- Chest X-Ray: An X-ray image of the chest can show whether the heart is enlarged and if there is fluid buildup in the lungs.
- Blood Tests: These tests check for markers of heart damage, infections, or other underlying conditions.
- Magnetic Resonance Imaging: An MRI provides detailed images of the heart and can help identify areas of damage or scarring.
- Cardiac Catheterization: This invasive procedure involves inserting a thin tube into a blood vessel to examine the heart’s arteries and measure pressure within the heart chambers.
Treatment and Care Options
While there is no cure for this condition, various treatments can help manage symptoms, slow disease progression, and improve quality of life. The treatment plan depends on the severity of the condition and the patient’s overall health.
Lifestyle Modifications
Making healthy lifestyle changes is often the first step in managing this condition:
- Healthy Diet: Consuming a balanced diet low in sodium, saturated fats, and processed foods can reduce strain on the heart.
- Regular Exercise: Engaging in light to moderate physical activity, as recommended by a doctor, can strengthen the heart and improve circulation.
- Weight Management: Maintaining a healthy weight reduces the workload on the heart.
- Limiting Alcohol and Tobacco: Avoiding excessive alcohol consumption and quitting smoking can prevent further damage to the heart.
Medications
Doctors may prescribe medications to alleviate symptoms and improve heart function:
- Beta-Blockers: These drugs slow the heart rate and reduce the heart’s workload.
- ACE Inhibitors: These medications lower blood pressure and improve blood flow.
- Diuretics: Often called water pills, these help reduce fluid buildup in the body.
- Anticoagulants: These medications prevent blood clots, reducing the risk of stroke.
Medical Procedures
In advanced cases, medical procedures may be necessary:
- Pacemaker Implantation: A device that helps regulate the heart’s rhythm.
- Implantable Cardioverter-Defibrillator: A device that monitors the heart and delivers shocks to restore normal rhythm if needed.
- Heart Transplant: For severe cases where other treatments have failed, a heart transplant may be considered.
Emotional and Mental Health Support
Living with this condition can take a toll on mental health. Patients may benefit from counseling, support groups, or therapy to cope with anxiety, depression, or stress related to their diagnosis.
Preventing Complications
Managing this condition requires ongoing care and vigilance. Regular follow-ups with a cardiologist are essential to monitor heart function and adjust treatment plans as needed. Patients should also be aware of warning signs that require immediate medical attention, such as severe chest pain, fainting, or sudden shortness of breath.
Tips for Long-Term Management
- Take medications as prescribed without skipping doses.
- Attend all scheduled appointments with healthcare providers.
- Monitor symptoms and report any changes promptly.
- Educate family members about the condition to ensure they can provide support during emergencies.