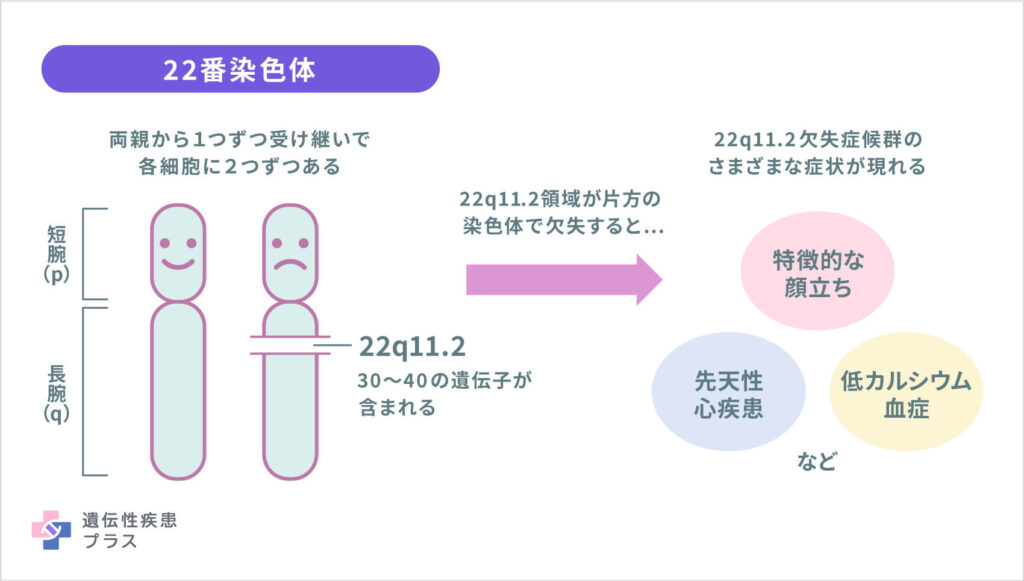
DiGeorge Syndrome, also known as 22q11.2 Deletion Syndrome, is a genetic disorder caused by the deletion of a small segment of chromosome 22. This condition affects multiple systems in the body and can lead to a wide range of physical, developmental, and behavioral challenges. Understanding its causes, symptoms, and care options is essential for individuals and families affected by this syndrome.
What is DiGeorge Syndrome?
DiGeorge Syndrome is a congenital disorder that occurs when a portion of chromosome 22 is missing. This deletion disrupts the normal development of various organs and systems in the body. The condition was first described by Dr. Angelo DiGeorge in the 1960s, and since then, significant progress has been made in understanding its underlying mechanisms and effects.
The missing genetic material impacts the development of structures derived from the third and fourth pharyngeal pouches during fetal growth. These structures include the thymus gland, parathyroid glands, and parts of the heart and facial structure. As a result, individuals with this condition may experience a variety of health issues.
Causes of DiGeorge Syndrome
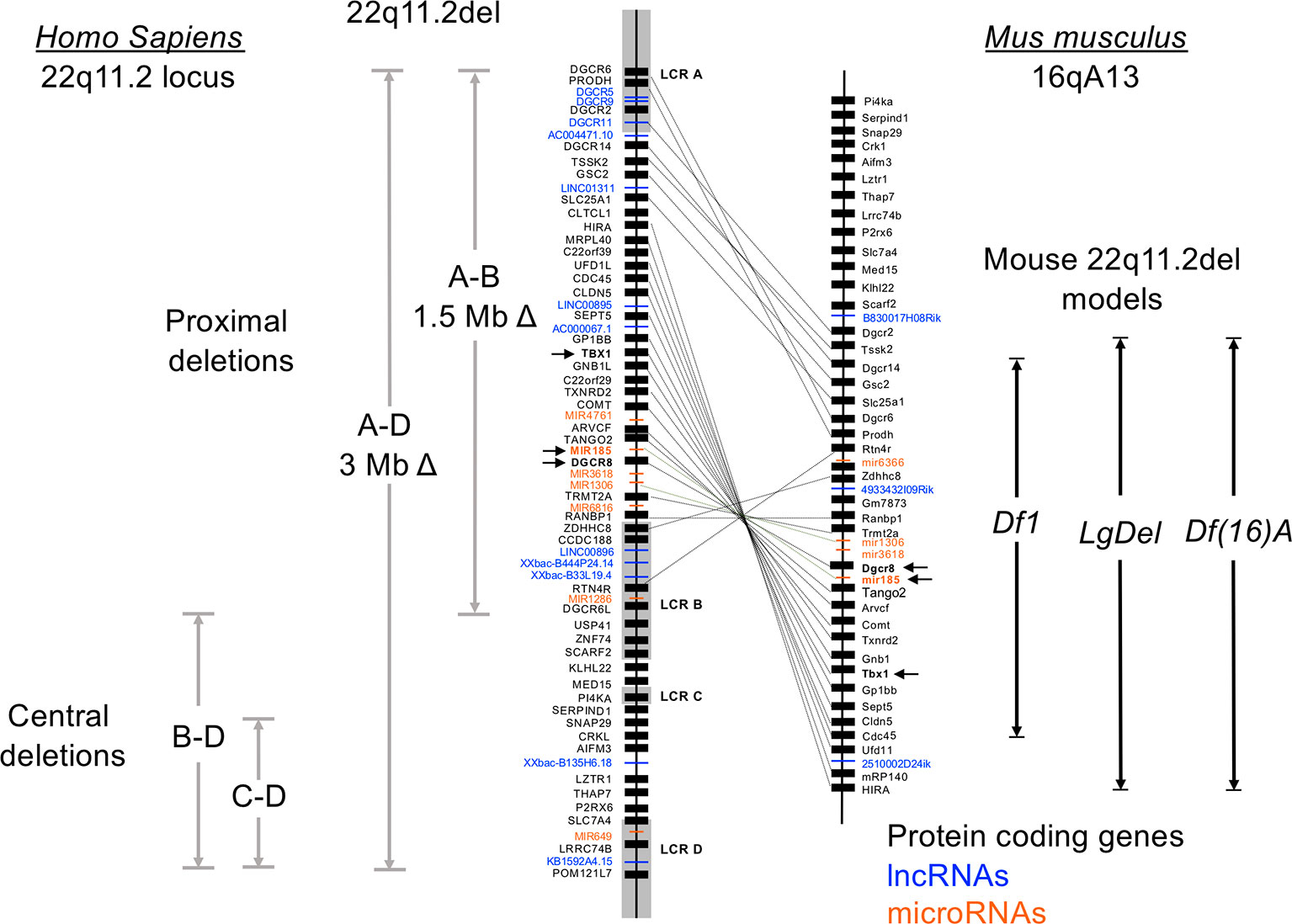
The primary cause of DiGeorge Syndrome is a spontaneous deletion of genetic material on chromosome 22. In most cases, this deletion occurs randomly during the formation of reproductive cells or in early fetal development. It is not typically inherited from parents, although there are rare instances where the deletion is passed down through families.
Researchers believe that the deletion affects the function of several genes, leading to the diverse symptoms observed in affected individuals. The loss of specific genes disrupts critical processes such as immune system development, calcium regulation, and cardiovascular formation.
Symptoms of DiGeorge Syndrome
The symptoms of DiGeorge Syndrome can vary widely among individuals. Some people may experience mild effects, while others face more severe challenges. The following sections outline the common symptoms associated with this condition.
Physical Symptoms
- Congenital Heart Defects: Many individuals with DiGeorge Syndrome are born with structural abnormalities in the heart, such as tetralogy of Fallot or interrupted aortic arch. These defects often require surgical intervention.
- Hypoparathyroidism: The parathyroid glands, which regulate calcium levels in the body, may be underdeveloped or absent. This can lead to low calcium levels, resulting in muscle cramps, seizures, and other complications.
- Distinct Facial Features: People with this condition may have characteristic facial features, including a small jaw, wide-set eyes, a cleft palate, or low-set ears.
Immune System Challenges
- Thymus Gland Abnormalities: The thymus plays a crucial role in the development of T-cells, which are essential for fighting infections. A poorly developed or absent thymus can lead to immunodeficiency, making individuals more susceptible to infections.
- Recurrent Infections: Due to a weakened immune system, individuals may experience frequent respiratory, ear, or sinus infections.
Developmental and Behavioral Symptoms
- Learning Disabilities: Many individuals with DiGeorge Syndrome experience delays in reaching developmental milestones. They may struggle with speech, language, and motor skills.
- Attention Deficit Hyperactivity Disorder (ADHD): ADHD is commonly observed in children with this condition, affecting their ability to focus and regulate behavior.
- Autism Spectrum Disorders: There is an increased prevalence of autism spectrum disorders among individuals with DiGeorge Syndrome, contributing to social and communication challenges.
Other Associated Conditions
- Kidney Abnormalities: Structural issues with the kidneys, such as cysts or malformations, may occur in some individuals.
- Gastrointestinal Problems: Feeding difficulties, constipation, and other digestive issues are common in infants and young children with this condition.
- Mental Health Concerns: Anxiety, depression, and other mental health conditions may arise due to the challenges associated with living with this syndrome.
Diagnosis of DiGeorge Syndrome
Diagnosing DiGeorge Syndrome typically involves a combination of clinical evaluations, imaging studies, and genetic testing. Early diagnosis is crucial for managing symptoms and providing appropriate care.
Clinical Evaluation
A healthcare provider may suspect DiGeorge Syndrome based on physical examination findings, such as characteristic facial features or signs of congenital heart defects. A detailed medical history and assessment of developmental milestones can also provide valuable clues.
Genetic Testing
Fluorescence in situ hybridization (FISH) is a commonly used test to detect the deletion on chromosome 22. More advanced techniques, such as chromosomal microarray analysis, can provide additional information about the extent of the deletion and its potential impact.
Additional Tests
Depending on the symptoms present, additional tests may be necessary to evaluate the function of the heart, immune system, and other organs. These may include echocardiograms, blood tests to measure calcium levels, and imaging studies to assess kidney and brain structure.
Treatment and Care for DiGeorge Syndrome
There is no cure for DiGeorge Syndrome, but comprehensive care can help manage symptoms and improve quality of life. Treatment plans are tailored to address the specific needs of each individual and often involve a multidisciplinary team of specialists.
Management of Congenital Heart Defects
Heart defects are one of the most serious complications of DiGeorge Syndrome. Surgical interventions, such as repairing structural abnormalities or implanting devices to support heart function, may be required. Regular monitoring by a cardiologist is essential to ensure optimal heart health.
Calcium and Parathyroid Support
Individuals with hypoparathyroidism require lifelong management of calcium and vitamin D levels. Oral supplements and dietary adjustments can help prevent complications such as seizures and muscle spasms. Regular blood tests are necessary to monitor calcium levels and adjust treatment as needed.
Immune System Support
For those with significant immune system deficiencies, treatments such as thymus transplants or immunoglobulin therapy may be considered. Preventive measures, including vaccinations and avoiding exposure to infections, are also important for maintaining health.
Developmental and Educational Interventions
Early intervention programs can play a vital role in addressing developmental delays and learning disabilities. Speech therapy, occupational therapy, and special education services can help children reach their full potential. Behavioral therapies may also be beneficial for managing ADHD or autism-related challenges.
Mental Health Support
Addressing mental health concerns is an integral part of care for individuals with DiGeorge Syndrome. Counseling, cognitive-behavioral therapy, and medication may be recommended to manage anxiety, depression, or other psychological issues.
Family and Community Support
Families of individuals with DiGeorge Syndrome often benefit from connecting with support groups and advocacy organizations. These resources provide valuable information, emotional support, and opportunities to connect with others facing similar challenges.
Living with DiGeorge Syndrome
Living with DiGeorge Syndrome requires ongoing medical care and attention to various aspects of health and well-being. While the condition presents unique challenges, many individuals with this syndrome lead fulfilling lives with the right support and interventions.
Transition to Adulthood
As children with DiGeorge Syndrome grow into adulthood, transitioning to adult healthcare providers and services becomes an important consideration. Planning for this transition early can help ensure continuity of care and address evolving needs.
Advances in Research
Ongoing research into the genetic and molecular basis of DiGeorge Syndrome holds promise for improved treatments and outcomes. Scientists are exploring potential therapies to address the root causes of the condition and mitigate its effects.