Diabetic retinopathy, often abbreviated as DR, is a serious complication of diabetes that affects the eyes. It occurs when high blood sugar levels cause damage to the blood vessels in the retina, leading to vision impairment or even blindness if left untreated. This condition is one of the leading causes of blindness among adults worldwide, making it crucial for individuals with diabetes to understand its causes, recognize its symptoms, and seek timely diagnosis and treatment. In this article, we will explore the underlying causes, common symptoms, diagnostic methods, and available treatments for diabetic retinopathy.
Understanding the Causes of Diabetic Retinopathy
Diabetic retinopathy develops as a result of prolonged high blood sugar levels damaging the delicate blood vessels in the retina. The retina is the light-sensitive tissue at the back of the eye responsible for converting light into signals that are sent to the brain, enabling us to see. When these blood vessels are damaged, they can leak fluid or bleed, causing swelling and impairing vision. Over time, the body may attempt to repair the damage by forming new blood vessels, but these new vessels are often weak and prone to leaking, further worsening the condition.
Prolonged Diabetes
The longer a person has diabetes, the higher their risk of developing diabetic retinopathy. Both Type 1 and Type 2 diabetes can lead to this condition, but the risk increases significantly if blood sugar levels are poorly managed over time. Consistently high blood sugar levels create an environment where the blood vessels in the retina become fragile and susceptible to damage.
Hypertension and High Cholesterol
In addition to diabetes, other health conditions such as hypertension (high blood pressure) and high cholesterol can exacerbate the risk of diabetic retinopathy. Hypertension places additional stress on the blood vessels, making them more likely to weaken and leak. Similarly, high cholesterol can contribute to the buildup of fatty deposits in the blood vessels, further restricting blood flow to the retina.
Pregnancy and Diabetic Retinopathy
Pregnancy can also pose a risk for women with diabetes. Hormonal changes during pregnancy may accelerate the progression of diabetic retinopathy, especially if blood sugar levels are not carefully monitored and controlled. Pregnant women with diabetes are often advised to undergo regular eye exams to detect any early signs of retinal damage.
Recognizing the Symptoms of Diabetic Retinopathy
One of the challenges of diabetic retinopathy is that it often progresses without noticeable symptoms in its early stages. By the time symptoms become apparent, significant damage may have already occurred. Therefore, understanding the potential warning signs is essential for early detection and intervention.
Blurred Vision
One of the earliest symptoms of diabetic retinopathy is blurred vision. This occurs when the macula, the central part of the retina responsible for sharp vision, becomes swollen due to fluid leakage from damaged blood vessels. Blurred vision can make it difficult to read, drive, or perform other daily activities.
Floating Spots or Dark Strings
Some individuals with diabetic retinopathy may notice floating spots or dark strings in their field of vision. These floaters are caused by tiny specks of blood that leak from damaged blood vessels in the retina. While floaters can sometimes resolve on their own, their presence should always be evaluated by an eye care professional.
Vision Loss
In advanced stages of diabetic retinopathy, vision loss can occur. This happens when extensive damage to the retina leads to scarring or detachment of the retina from the back of the eye. Once vision loss occurs, it may be irreversible, highlighting the importance of early detection and treatment.
Diagnosing Diabetic Retinopathy
Early diagnosis is critical for preventing vision loss caused by diabetic retinopathy. Regular eye exams are essential for individuals with diabetes, as they allow eye care professionals to detect retinal damage before symptoms become severe. Several diagnostic methods are used to identify and monitor diabetic retinopathy.
Dilated Eye Exam
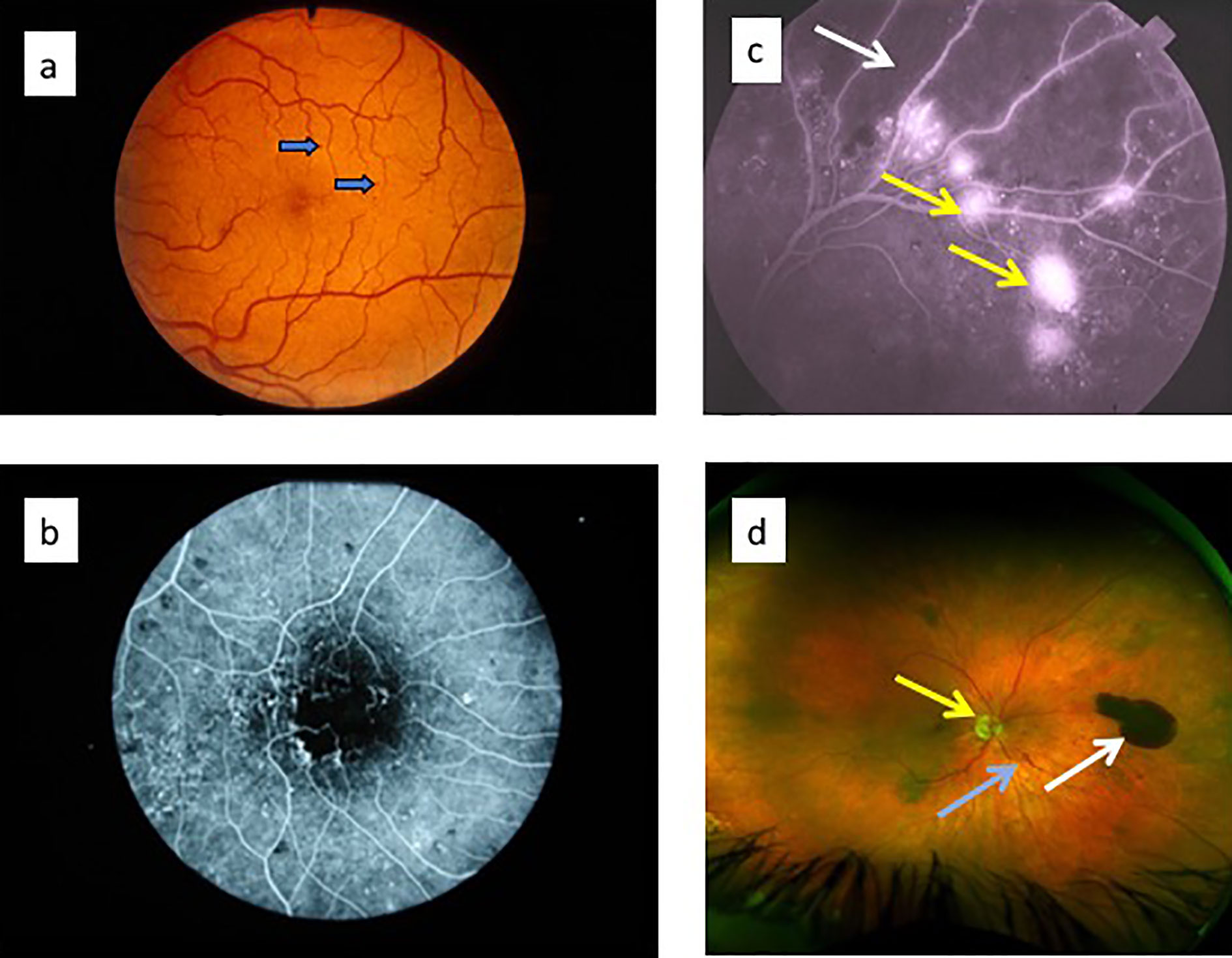
A dilated eye exam is one of the most common diagnostic tools for diabetic retinopathy. During this exam, an eye care professional administers eye drops to dilate the pupils, allowing them to examine the retina and optic nerve for signs of damage. They look for abnormalities such as swelling, leaking blood vessels, or the growth of new, abnormal blood vessels.
Fluorescein Angiography
Fluorescein angiography is another diagnostic test used to evaluate the blood vessels in the retina. During this procedure, a special dye is injected into a vein in the arm. As the dye travels through the bloodstream, it highlights the blood vessels in the retina, allowing the doctor to identify areas of leakage or blockage.
Optical Coherence Tomography
Optical coherence tomography is a non-invasive imaging test that provides detailed cross-sectional images of the retina. This test is particularly useful for detecting swelling in the macula, which is a common complication of diabetic retinopathy. It can also help monitor the effectiveness of treatments over time.
Treatment Options for Diabetic Retinopathy
While diabetic retinopathy cannot be cured, several treatment options are available to slow its progression and prevent vision loss. The choice of treatment depends on the severity of the condition and the specific needs of the patient.
Laser Treatment
Laser treatment, also known as photocoagulation, is a common procedure used to treat diabetic retinopathy. During this procedure, a laser is used to seal leaking blood vessels or destroy abnormal blood vessels in the retina. Laser treatment can help reduce swelling in the retina and prevent further damage, although it may not restore lost vision.
Vitrectomy
In cases where there is significant bleeding or scarring in the retina, a surgical procedure called vitrectomy may be necessary. During a vitrectomy, the gel-like substance inside the eye, known as the vitreous, is removed and replaced with a clear solution. This allows the surgeon to repair any damage to the retina and remove scar tissue that may be pulling on the retina.
Anti-VEGF Injections
Anti-vascular endothelial growth factor injections are another treatment option for diabetic retinopathy. These injections work by blocking the growth of abnormal blood vessels in the retina and reducing swelling. Anti-VEGF injections are typically administered directly into the eye and may require multiple treatments over time.
Blood Sugar and Blood Pressure Management
- Blood Sugar Control: One of the most effective ways to manage diabetic retinopathy is through tight control of blood sugar levels. Maintaining stable blood sugar levels can slow the progression of the disease and reduce the risk of complications.
- Blood Pressure Management: Controlling blood pressure is equally important, as high blood pressure can worsen retinal damage. Lifestyle changes such as adopting a healthy diet, exercising regularly, and taking prescribed medications can help keep blood pressure within a healthy range.
Preventive Measures for Diabetic Retinopathy
While treatment is essential for managing diabetic retinopathy, prevention plays an equally important role in protecting vision. By adopting healthy habits and staying vigilant about regular eye exams, individuals with diabetes can reduce their risk of developing this condition.
Regular Eye Exams
Individuals with diabetes should schedule comprehensive eye exams at least once a year, even if they are not experiencing any symptoms. Early detection of retinal damage allows for timely intervention and better outcomes.
Healthy Lifestyle Choices
Making healthy lifestyle choices can significantly lower the risk of diabetic retinopathy. These include maintaining a balanced diet rich in fruits, vegetables, and whole grains, engaging in regular physical activity, and avoiding smoking. These habits not only support overall health but also help regulate blood sugar and blood pressure levels.
Monitoring Blood Sugar Levels
Regular monitoring of blood sugar levels is crucial for preventing complications associated with diabetes, including diabetic retinopathy. By keeping blood sugar levels within the target range recommended by a healthcare provider, individuals can minimize the risk of damage to the blood vessels in the retina.





