Diabetes is a chronic condition that affects millions of people worldwide. Among its many complications, Peripheral Neuropathy (PN) stands out as one of the most common and debilitating issues. This condition refers to damage to the peripheral nerves, which are responsible for transmitting signals between the central nervous system and the rest of the body. Understanding the causes, recognizing the symptoms, and adopting proper care strategies are essential for managing this complication effectively.
Understanding Peripheral Nerve Damage
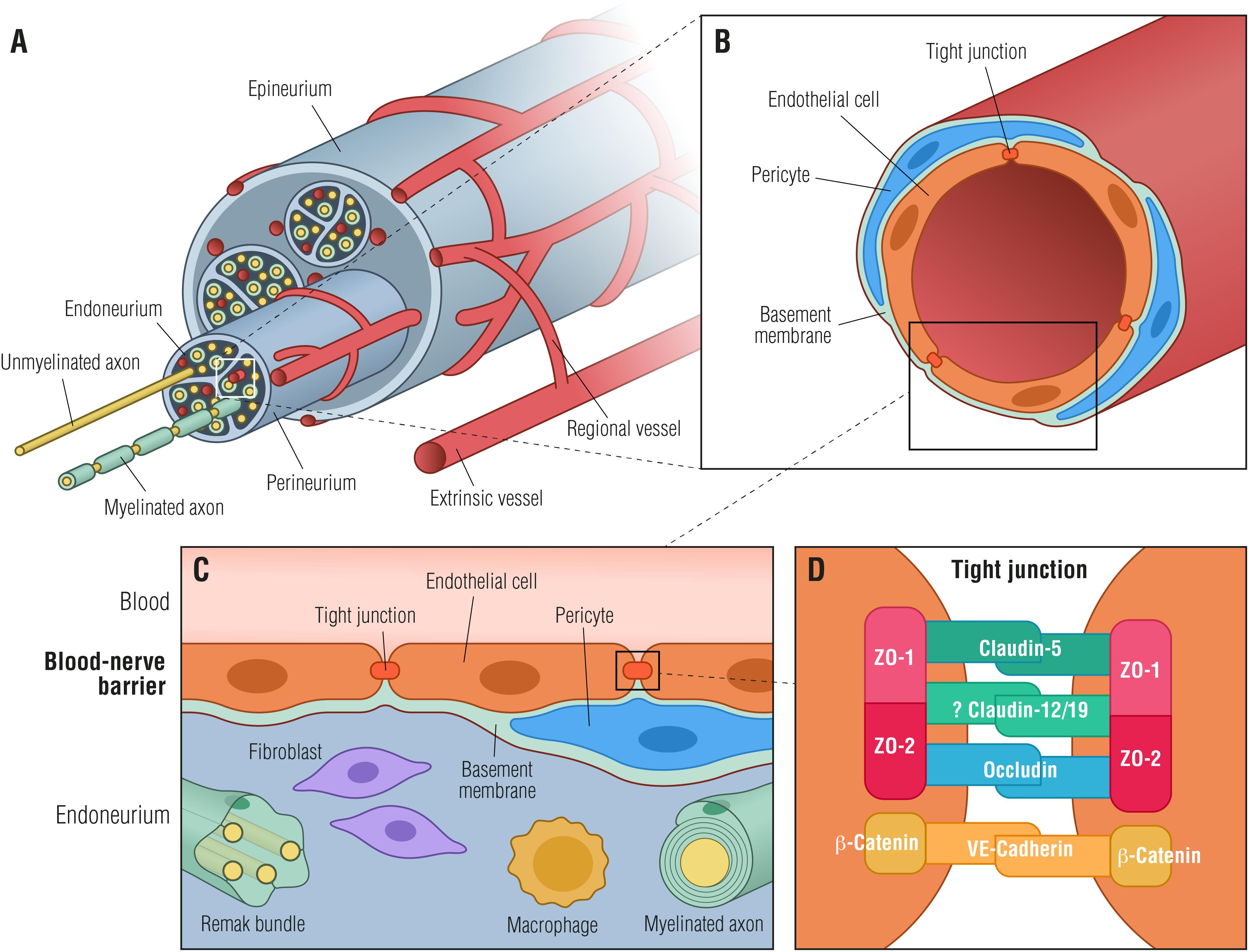
Peripheral nerve damage occurs when the nerves outside of the brain and spinal cord are impaired or destroyed. In individuals with diabetes, high blood sugar levels over time can lead to nerve damage. The peripheral nerves play a crucial role in controlling movement, sensation, and even some involuntary functions like digestion and heart rate. When these nerves are damaged, it can result in a wide range of symptoms and complications.
Types of Peripheral Nerve Damage
- Sensory Nerve Damage: Affects the ability to feel pain, temperature, and touch.
- Motor Nerve Damage: Impairs muscle control and coordination.
- Autonomic Nerve Damage: Disrupts the regulation of involuntary bodily functions such as digestion and blood pressure.
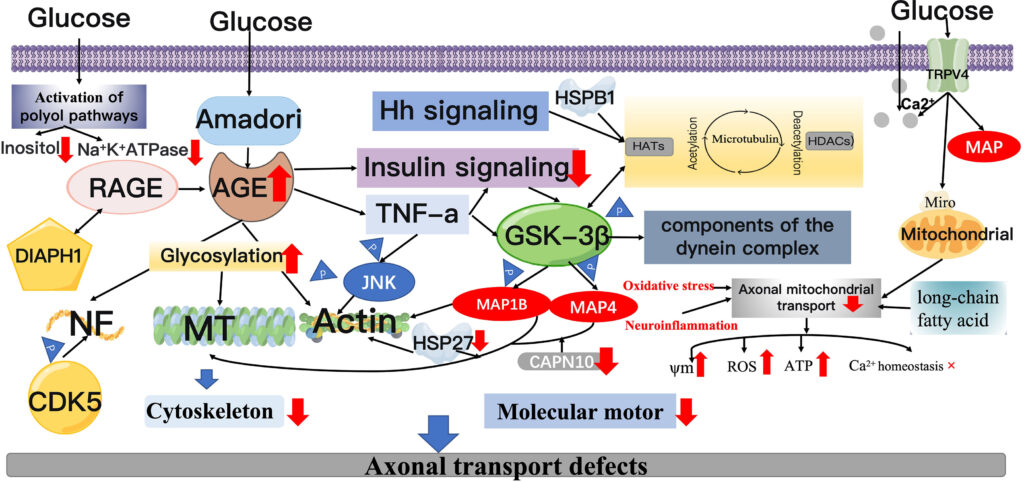
Causes of Peripheral Nerve Damage in Diabetes
The exact mechanisms behind nerve damage in diabetes are complex and not fully understood. However, several factors contribute to this condition.
Prolonged High Blood Sugar Levels
One of the primary causes of nerve damage in diabetes is prolonged exposure to high blood sugar levels. Elevated glucose levels can interfere with the nerves’ ability to transmit signals. Additionally, high blood sugar can damage the small blood vessels that supply oxygen and nutrients to the nerves, leading to their deterioration over time.
Inflammation and Oxidative Stress
Chronic inflammation and oxidative stress are also significant contributors to nerve damage. High blood sugar levels can trigger an inflammatory response in the body, causing damage to nerve tissues. Oxidative stress, which occurs when there is an imbalance between free radicals and antioxidants in the body, can further exacerbate nerve damage by harming cellular components.
Genetic Factors
Some individuals may be genetically predisposed to developing nerve damage. Certain genetic factors can make nerves more susceptible to injury from high blood sugar levels, increasing the risk of peripheral neuropathy.
Symptoms of Peripheral Nerve Damage
The symptoms of peripheral nerve damage can vary depending on the type of nerves affected and the severity of the condition. These symptoms often develop gradually and may go unnoticed in the early stages.
Sensory Symptoms
- Numbness or reduced ability to feel pain or temperature changes, especially in the feet and hands.
- Tingling or burning sensations.
- Sharp, jabbing, or throbbing pain.
- Increased sensitivity to touch.
Motor Symptoms
- Muscle weakness or loss of coordination.
- Difficulty walking or performing tasks that require fine motor skills.
- Muscle wasting in severe cases.
Autonomic Symptoms
- Digestive issues such as nausea, vomiting, diarrhea, or constipation.
- Problems with bladder control.
- Changes in blood pressure, leading to dizziness or fainting.
- Irregular heart rate.
Risk Factors for Developing Peripheral Nerve Damage
While diabetes itself is a significant risk factor for peripheral nerve damage, other factors can increase the likelihood of developing this condition.
Duration of Diabetes
The longer someone has diabetes, the higher their risk of developing nerve damage. Over time, the cumulative effects of high blood sugar levels can take a toll on nerve health.
Poor Blood Sugar Control
Individuals who struggle to maintain stable blood sugar levels are at a greater risk of nerve damage. Consistently high blood sugar levels accelerate the progression of nerve damage.
Other Health Conditions
Certain health conditions, such as kidney disease, can exacerbate nerve damage. Kidney disease can lead to the accumulation of toxins in the blood, which can further harm nerve tissues.
Diagnosing Peripheral Nerve Damage
Early diagnosis of peripheral nerve damage is crucial for preventing further complications. Healthcare providers use a combination of methods to diagnose this condition.
Physical Examination
A thorough physical examination can help identify signs of nerve damage. During the exam, the healthcare provider may check for numbness, muscle weakness, and changes in reflexes.
Neurological Tests
Various neurological tests can assess nerve function. These may include tests to measure the speed and strength of nerve signals, as well as tests to evaluate sensory perception.
Imaging and Laboratory Tests
In some cases, imaging studies such as magnetic resonance imaging or computed tomography scans may be used to rule out other causes of symptoms. Blood tests can also help identify underlying conditions that may contribute to nerve damage.
Treatment Options for Peripheral Nerve Damage
While there is no cure for peripheral nerve damage, several treatment options can help manage symptoms and slow the progression of the condition.
Blood Sugar Management
The cornerstone of treatment for nerve damage in diabetes is maintaining tight control over blood sugar levels. Keeping blood sugar within a target range can prevent further nerve damage and improve overall health outcomes.
Medications
Several medications can help alleviate the symptoms of nerve damage. Pain relievers, both over-the-counter and prescription, can help manage discomfort. Antidepressants and anticonvulsants are also commonly prescribed to treat nerve pain.
Physical Therapy
Physical therapy can help improve muscle strength and coordination. Exercises tailored to the individual’s needs can enhance mobility and reduce the risk of falls.
Lifestyle Modifications
Making certain lifestyle changes can also have a positive impact on nerve health. Regular exercise, a balanced diet, and avoiding smoking and excessive alcohol consumption can all contribute to better nerve function.
Preventing Peripheral Nerve Damage
Prevention is key to avoiding the complications associated with peripheral nerve damage. By taking proactive steps, individuals with diabetes can reduce their risk of developing this condition.
Regular Monitoring
Regular monitoring of blood sugar levels is essential for preventing nerve damage. Frequent testing can help individuals stay aware of their blood sugar trends and make necessary adjustments to their treatment plan.
Foot Care
Proper foot care is critical for individuals with diabetes. Regularly inspecting the feet for cuts, blisters, or sores can help prevent infections and complications. Wearing comfortable, well-fitting shoes and keeping the feet clean and moisturized is also important.
Healthy Diet and Exercise
A healthy diet rich in fruits, vegetables, whole grains, and lean proteins can support nerve health. Regular exercise can improve circulation and promote overall well-being, reducing the risk of nerve damage.
Living with Peripheral Nerve Damage
Living with peripheral nerve damage can be challenging, but with the right strategies, individuals can manage their symptoms and maintain a good quality of life.
Support Systems
Building a strong support system is essential for coping with the emotional and physical challenges of nerve damage. Support groups, counseling, and open communication with healthcare providers can provide valuable resources and encouragement.
Adaptive Devices
Using adaptive devices such as braces, canes, or specialized footwear can help individuals with nerve damage maintain independence and mobility. These tools can compensate for muscle weakness and balance issues, reducing the risk of falls.
Education and Awareness
Staying informed about peripheral nerve damage and its management is crucial for individuals with diabetes. Understanding the condition and its potential complications can empower individuals to take an active role in their care.