Diabetes Insipidus, often abbreviated as DI, is a rare medical condition that affects the body’s ability to regulate fluid balance. Unlike diabetes mellitus, which involves issues with blood sugar regulation, this condition is characterized by excessive thirst and the production of large amounts of diluted urine. Understanding the types, causes, symptoms, and treatments of this disorder is essential for managing it effectively and improving the quality of life for those affected.

What Is Diabetes Insipidus?
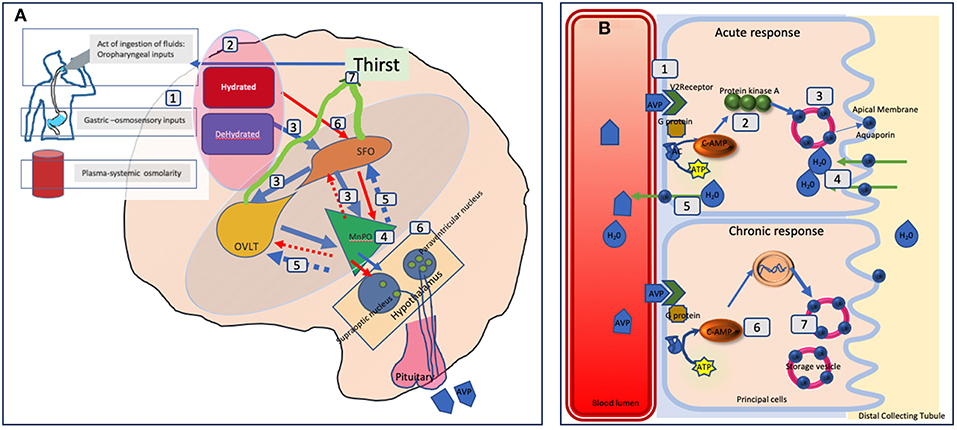
Diabetes Insipidus is a disorder of water metabolism that disrupts the normal functioning of antidiuretic hormone, also known as vasopressin. This hormone plays a crucial role in maintaining the balance of water in the body by controlling how much water is reabsorbed by the kidneys. When this process is disrupted, the kidneys are unable to concentrate urine properly, leading to excessive urination and dehydration.
How Does It Differ from Diabetes Mellitus?
While both conditions share the name “diabetes,” they are entirely different. Diabetes mellitus involves problems with insulin and glucose metabolism, leading to high blood sugar levels. In contrast, Diabetes Insipidus is related to the regulation of water in the body and does not involve blood sugar abnormalities. The confusion between the two arises because both conditions cause increased thirst and frequent urination, but their underlying mechanisms and treatments differ significantly.
Types of Diabetes Insipidus
There are four main types of Diabetes Insipidus, each with distinct causes and characteristics. Understanding these types is essential for accurate diagnosis and treatment.
Central Diabetes Insipidus
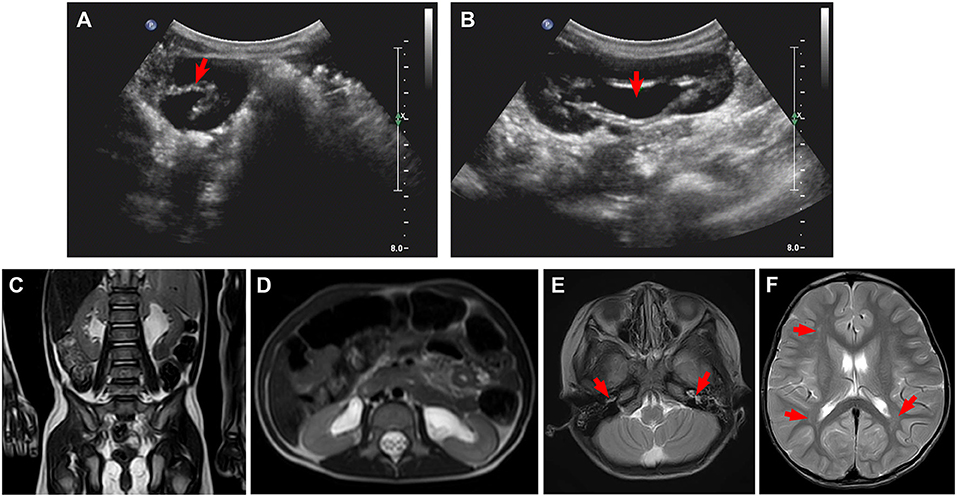
Central Diabetes Insipidus occurs when the body does not produce enough antidiuretic hormone. This type is often caused by damage to the hypothalamus or pituitary gland, which are responsible for producing and releasing the hormone. Common causes include head injuries, tumors, infections, or surgical procedures involving the brain.
Nephrogenic Diabetes Insipidus
In Nephrogenic Diabetes Insipidus, the kidneys fail to respond properly to the antidiuretic hormone, even though the hormone is present in adequate amounts. This can result from genetic mutations, chronic kidney disease, certain medications like lithium, or electrolyte imbalances such as high calcium or low potassium levels.
Gestational Diabetes Insipidus
Gestational Diabetes Insipidus is a rare form that occurs during pregnancy. It happens when an enzyme produced by the placenta breaks down the antidiuretic hormone, leading to symptoms similar to other types of this condition. Fortunately, this type usually resolves after childbirth.
Dipsogenic Diabetes Insipidus
Dipsogenic Diabetes Insipidus is caused by excessive fluid intake, which suppresses the release of antidiuretic hormone. This type is often linked to underlying conditions such as mental health disorders, certain medications, or damage to the thirst-regulating mechanism in the brain.
Causes of Diabetes Insipidus
The causes of Diabetes Insipidus vary depending on the type. Identifying the root cause is critical for determining the appropriate treatment plan.
Damage to the Hypothalamus or Pituitary Gland
In Central Diabetes Insipidus, damage to the hypothalamus or pituitary gland is a primary cause. This damage can occur due to:
- Traumatic brain injuries
- Tumors or cysts in the brain
- Infections such as meningitis or encephalitis
- Surgical procedures involving the brain
- Radiation therapy targeting the brain
Kidney Dysfunction
Nephrogenic Diabetes Insipidus is often caused by conditions that impair the kidneys’ ability to respond to antidiuretic hormone. These include:
- Chronic kidney disease
- Genetic mutations affecting kidney function
- Medications such as lithium or certain diuretics
- Electrolyte imbalances like hypercalcemia or hypokalemia
Hormonal Changes During Pregnancy
Gestational Diabetes Insipidus is triggered by hormonal changes during pregnancy. The placenta produces an enzyme called vasopressinase, which breaks down antidiuretic hormone. This condition is typically temporary and resolves after delivery.
Excessive Fluid Intake
Dipsogenic Diabetes Insipidus results from drinking excessive amounts of fluids, which can suppress the release of antidiuretic hormone. This may be caused by:
- Mental health conditions such as psychogenic polydipsia
- Certain medications that increase thirst
- Damage to the thirst-regulating center in the brain
Symptoms of Diabetes Insipidus
The symptoms of Diabetes Insipidus are similar across all types and primarily revolve around excessive urination and thirst. Recognizing these symptoms early can help in seeking timely medical intervention.
Excessive Urination
One of the hallmark symptoms is the production of large volumes of diluted urine. Individuals may urinate frequently throughout the day and night, disrupting sleep patterns and daily activities.
Intense Thirst
Due to the loss of fluids through excessive urination, individuals experience intense thirst and a constant need to drink water. This can lead to consuming large amounts of fluids in an attempt to stay hydrated.
Dehydration
If fluid intake does not match the amount lost through urination, dehydration can occur. Signs of dehydration include dry mouth, fatigue, dizziness, and confusion.
Other Symptoms
In severe cases, untreated Diabetes Insipidus can lead to complications such as:
- Electrolyte imbalances
- Weight loss
- Irritability and mood changes
- Low blood pressure
Treatments for Diabetes Insipidus
The treatment for Diabetes Insipidus depends on the type and underlying cause. While there is no cure for most forms of this condition, effective management strategies can help control symptoms and improve quality of life.
Treatment for Central Diabetes Insipidus
For Central Diabetes Insipidus, the primary treatment involves replacing the deficient antidiuretic hormone. A synthetic version of the hormone, known as desmopressin, is commonly prescribed. This medication can be administered as a nasal spray, injection, or oral tablet and helps reduce urine production and alleviate symptoms.
Treatment for Nephrogenic Diabetes Insipidus
Treating Nephrogenic Diabetes Insipidus focuses on addressing the underlying cause. For example:
- Adjusting or discontinuing medications that impair kidney function
- Correcting electrolyte imbalances through diet or supplements
- Managing chronic kidney disease with appropriate therapies
In some cases, medications like thiazide diuretics or nonsteroidal anti-inflammatory drugs may be used to reduce urine output.
Treatment for Gestational Diabetes Insipidus
Gestational Diabetes Insipidus is typically managed with desmopressin to replace the deficient hormone. Since this condition is temporary, treatment is usually discontinued after childbirth once hormone levels return to normal.
Treatment for Dipsogenic Diabetes Insipidus
Managing Dipsogenic Diabetes Insipidus involves addressing the underlying cause of excessive fluid intake. Treatment options may include:
- Behavioral therapy for individuals with psychogenic polydipsia
- Adjusting medications that increase thirst
- Treating any neurological conditions affecting thirst regulation
Living with Diabetes Insipidus
Living with Diabetes Insipidus requires careful monitoring and lifestyle adjustments to manage symptoms effectively. Staying hydrated, following a balanced diet, and adhering to prescribed treatments are essential steps for maintaining overall health.
Importance of Regular Medical Checkups
Regular follow-ups with healthcare providers are crucial for monitoring the condition and making necessary adjustments to the treatment plan. Blood tests, urine tests, and imaging studies may be performed periodically to assess kidney function and hormone levels.
Lifestyle Modifications
Individuals with Diabetes Insipidus can benefit from adopting healthy habits, such as:
- Drinking water in moderation to avoid overhydration or dehydration
- Avoiding caffeine and alcohol, which can exacerbate symptoms
- Maintaining a balanced diet rich in essential nutrients
Support Systems
Building a strong support system, including family, friends, and healthcare professionals, can make a significant difference in coping with the challenges of living with Diabetes Insipidus. Support groups and online communities can also provide valuable resources and encouragement.