A dental abscess, also known as a tooth abscess, is a serious oral health condition that requires prompt attention. Abbreviated as DA in medical records, it refers to a pocket of pus caused by a bacterial infection. This article will delve into the causes, symptoms, diagnosis, and treatment options for this painful condition.
What Is a Dental Abscess?
A dental abscess is a localized collection of pus that forms inside the teeth or gums. It typically occurs when bacteria invade the dental pulp, which is the innermost part of the tooth containing nerves, blood vessels, and connective tissue. The buildup of pus results from the body’s immune response to the infection, creating pressure and causing significant discomfort.
Types of Dental Abscesses
- Periapical Abscess: This type originates at the tip of the tooth’s root. It usually develops due to an untreated cavity or injury that allows bacteria to enter the pulp chamber.
- Periodontal Abscess: This abscess occurs in the gum tissue next to a tooth. It is often linked to advanced gum disease or trauma to the gums.
- Gingival Abscess: A gingival abscess is limited to the gum tissue and does not affect the tooth or its supporting structures.
Causes of Dental Abscess
Understanding the causes of a dental abscess can help prevent its occurrence. Several factors contribute to the development of this condition:
Poor Oral Hygiene
Inadequate brushing and flossing allow plaque, a sticky film of bacteria, to accumulate on the teeth. Over time, plaque hardens into tartar, leading to cavities and gum disease, both of which increase the risk of abscess formation.
Untreated Cavities
Cavities provide an entry point for bacteria to reach the inner layers of the tooth. If left untreated, the decay progresses, eventually reaching the pulp and causing an infection that may result in an abscess.
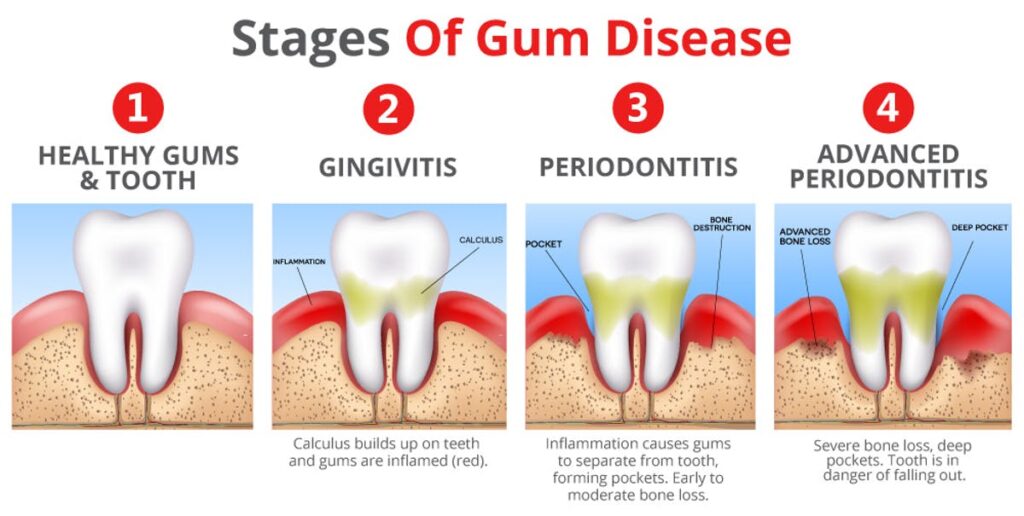
Gum Disease
Gum disease, also known as periodontal disease, weakens the structures supporting the teeth. Bacteria thrive in the pockets formed between the gums and teeth, potentially leading to a periodontal abscess.
Tooth Injury or Trauma
A cracked or chipped tooth can expose the dental pulp to bacteria, increasing the likelihood of infection. Similarly, trauma to the gums or surrounding tissues can create an environment conducive to abscess formation.
Weakened Immune System
Individuals with compromised immune systems, such as those with diabetes or undergoing chemotherapy, are more susceptible to infections, including dental abscesses.
Symptoms of Dental Abscess
The symptoms of a dental abscess can vary depending on its location and severity. Recognizing these signs early can facilitate timely treatment and prevent complications.
Severe Toothache
A persistent, throbbing pain in the affected tooth is one of the most common symptoms. The pain may radiate to the jaw, ear, or neck and worsen when lying down.
Sensitivity to Temperature
Individuals with a dental abscess often experience heightened sensitivity to hot or cold foods and beverages. This sensitivity is due to the inflammation of the dental pulp.
Swelling and Redness
Swelling in the face or cheek near the affected area is a telltale sign of an abscess. The gums may also appear red, swollen, and tender to the touch.
Fever and General Discomfort
A fever accompanied by fatigue or malaise may indicate that the infection has spread beyond the tooth or gum. This is a serious sign that warrants immediate medical attention.
Bad Taste or Smell
An unpleasant taste or odor in the mouth can occur if the abscess ruptures, releasing pus into the oral cavity.
Difficulty Chewing or Swallowing
The pain and swelling associated with a dental abscess can make it challenging to chew food or swallow properly.
Diagnosis of Dental Abscess
Diagnosing a dental abscess involves a combination of clinical evaluation and diagnostic tests. A dentist will assess the patient’s symptoms and perform a thorough examination to determine the underlying cause.
Physical Examination
During the physical examination, the dentist will inspect the mouth for visible signs of infection, such as swelling, redness, or pus drainage. They may also tap on the affected tooth to check for sensitivity.
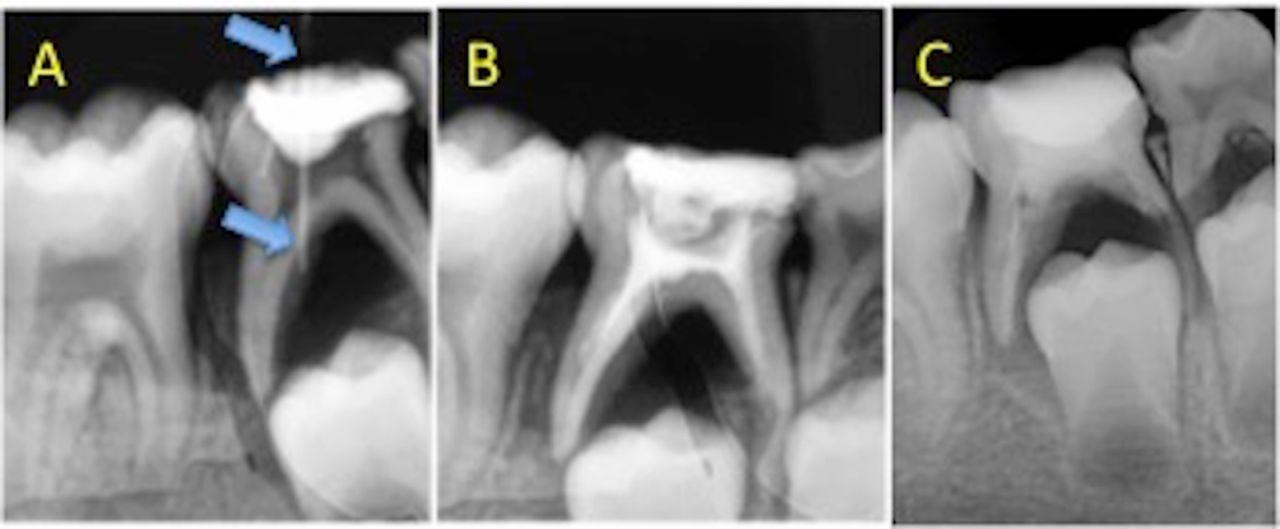
X-rays
Dental X-rays are essential for identifying the extent of the infection and locating the source of the abscess. These images reveal whether the infection has spread to nearby teeth, bones, or soft tissues.
CT Scan
In cases where the infection is severe or has spread, a computed tomography scan may be necessary to obtain a detailed view of the affected area. This imaging technique helps guide treatment decisions.
Microbiological Testing
In some instances, a sample of the pus may be collected and sent to a laboratory for analysis. This test identifies the specific bacteria causing the infection, allowing for targeted antibiotic therapy.
Treatment Options for Dental Abscess
The primary goal of treating a dental abscess is to eliminate the infection, preserve the affected tooth, and prevent complications. The treatment approach depends on the type and severity of the abscess.
Drainage of the Abscess
One of the first steps in treating a dental abscess is draining the pus. The dentist creates a small incision in the abscess to release the accumulated fluid, providing immediate relief from pain and pressure.
Root Canal Therapy
For periapical abscesses, root canal therapy is often recommended. This procedure involves removing the infected pulp, cleaning the inside of the tooth, and sealing it to prevent further infection. Root canal therapy can save the tooth and restore its function.
Tooth Extraction
If the tooth is severely damaged and cannot be saved, extraction may be necessary. Removing the tooth eliminates the source of the infection and allows the surrounding tissues to heal.
Antibiotics
Antibiotics are prescribed to control the spread of infection, especially in cases where the abscess has extended beyond the tooth or gum. Commonly used antibiotics include amoxicillin and metronidazole. However, antibiotics alone are not sufficient to cure a dental abscess; they must be combined with other treatments.
Pain Management
Pain relief is an important aspect of managing a dental abscess. Over-the-counter pain relievers such as ibuprofen or acetaminophen can help alleviate discomfort. In severe cases, prescription pain medications may be required.
Warm Salt Water Rinses
Rinsing the mouth with warm salt water several times a day can reduce swelling and promote healing. This simple home remedy also helps keep the mouth clean and free of bacteria.
Follow-Up Care
After initial treatment, regular follow-up visits are crucial to monitor the healing process and ensure that the infection does not recur. The dentist may recommend additional procedures, such as scaling and root planing, to address underlying gum disease.
Preventing Dental Abscess
While treatment is essential, prevention plays a key role in avoiding the development of a dental abscess. Adopting good oral hygiene practices and seeking timely dental care can significantly reduce the risk.
Maintain Proper Oral Hygiene
Brushing twice a day with fluoride toothpaste and flossing daily removes plaque and prevents cavities. Using an antibacterial mouthwash can further enhance oral health.
Visit the Dentist Regularly
Regular dental check-ups and professional cleanings help detect and address issues before they escalate into serious problems. Dentists can identify early signs of decay or gum disease and provide appropriate interventions.
Address Dental Issues Promptly
Seeking treatment for cavities, cracked teeth, or gum disease at the earliest stage prevents complications. Ignoring these problems increases the risk of abscess formation.
Eat a Balanced Diet
A diet rich in fruits, vegetables, and whole grains supports overall health, including oral health. Limiting sugary snacks and beverages reduces the risk of cavities and gum disease.
Protect Teeth from Injury
Wearing a mouthguard during sports or activities that pose a risk of dental trauma can prevent injuries that may lead to abscesses.