Degenerative disc disease, often abbreviated as DDD, is a common condition that affects the spine. It occurs when the discs between the vertebrae begin to break down, leading to pain and discomfort. This condition is not technically a disease but rather a natural part of aging for many people. However, it can significantly impact quality of life if left untreated or improperly managed. In this article, we will explore the causes, symptoms, and care options available for those dealing with degenerative disc disease.
What Is Degenerative Disc Disease?
Degenerative disc disease refers to the gradual deterioration of the spinal discs, which are the soft, gel-like structures located between the bones of the spine. These discs act as cushions, absorbing shock and allowing flexibility in the spine. Over time, these discs lose their water content, elasticity, and ability to function effectively. As a result, they become thinner, weaker, and more prone to damage.
While this process is a normal part of aging, some individuals experience more severe symptoms than others. The degree of discomfort and the specific areas affected can vary widely, depending on factors such as genetics, lifestyle, and overall health.
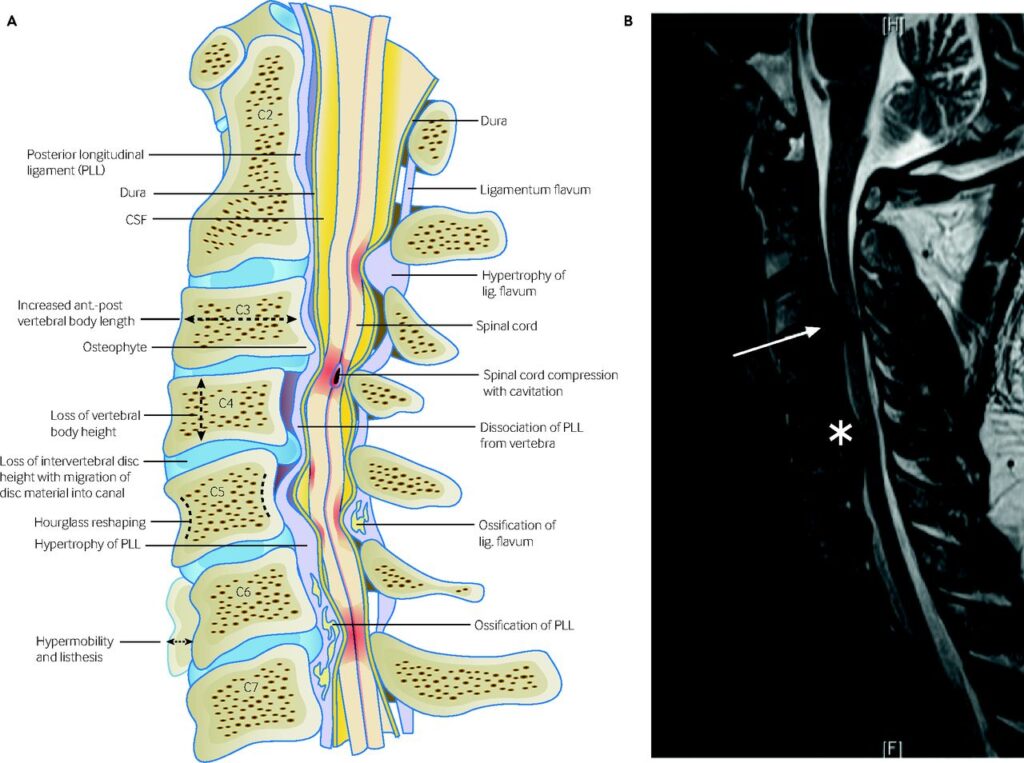
How Does It Affect the Spine?
The spine is made up of individual bones called vertebrae, which are separated by intervertebral discs. These discs play a critical role in maintaining the spine’s structure and mobility. When degeneration occurs, the following changes may happen:
- The outer layer of the disc, known as the annulus fibrosus, may develop small tears or cracks.
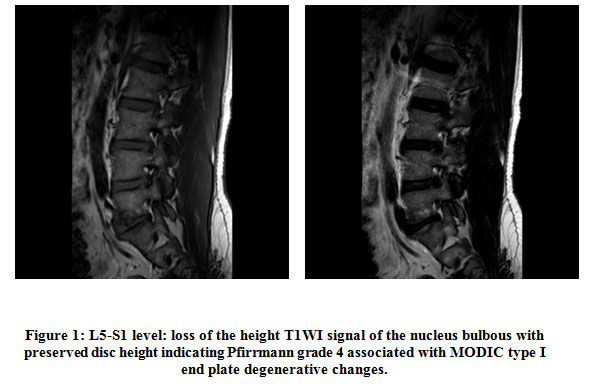
- The inner core of the disc, called the nucleus pulposus, may lose its ability to retain water, making it less effective as a shock absorber.
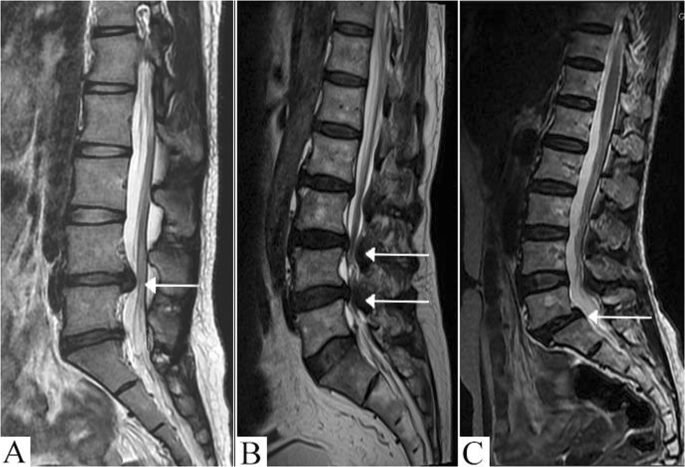
- The disc may bulge or herniate, pressing on nearby nerves and causing pain.
- Bone spurs may form as the body attempts to stabilize the affected area, potentially leading to further complications.
Causes of Degenerative Disc Disease
Several factors contribute to the development of degenerative disc disease. While aging is the primary cause, other elements can accelerate the process or increase the risk of experiencing symptoms.
Aging
As people grow older, their bodies undergo various changes, including the gradual wear and tear of the spinal discs. Over time, the discs lose hydration and elasticity, making them more susceptible to damage. This natural process begins as early as the second decade of life and progresses gradually.
Injury or Trauma
Injuries to the spine, such as those caused by accidents, falls, or sports-related activities, can accelerate disc degeneration. Even minor injuries can lead to long-term damage if not properly treated. Additionally, repetitive stress on the spine, such as heavy lifting or poor posture, can contribute to the breakdown of the discs.
Genetics
Some individuals are genetically predisposed to developing degenerative disc disease. If a close family member has experienced similar issues, there may be an increased likelihood of inheriting a predisposition to disc degeneration.
Lifestyle Factors
Certain lifestyle choices can exacerbate the progression of degenerative disc disease. These include:
- Smoking: Smoking reduces blood flow to the discs, depriving them of essential nutrients and oxygen.
- Obesity: Excess weight places additional strain on the spine, accelerating wear and tear.
- Sedentary Lifestyle: Lack of physical activity can weaken the muscles supporting the spine, increasing the risk of disc problems.
Symptoms of Degenerative Disc Disease
The symptoms of degenerative disc disease can vary widely from person to person. Some individuals may experience mild discomfort, while others may face debilitating pain. Common symptoms include:
Pain
Pain is the most prevalent symptom of degenerative disc disease. It often occurs in the lower back or neck, depending on the location of the affected discs. The pain may:
- Be intermittent or constant.
- Worsen with certain activities, such as bending, lifting, or twisting.
- Improve with rest or changing positions.
Numbness or Tingling
If a degenerated disc presses on a nerve, it can cause numbness or tingling sensations in the arms, legs, hands, or feet. This is often referred to as radiculopathy and can significantly impact daily activities.
Muscle Weakness
In severe cases, nerve compression can lead to muscle weakness in the affected area. For example, individuals may notice difficulty gripping objects or walking steadily.
Stiffness
Many people with degenerative disc disease report stiffness in the spine, particularly in the morning or after periods of inactivity. This stiffness can make movement challenging and uncomfortable.
Care Options for Degenerative Disc Disease
There are several approaches to managing degenerative disc disease, ranging from conservative treatments to surgical interventions. The choice of care depends on the severity of symptoms, the location of the affected discs, and the individual’s overall health.
Non-Surgical Treatments
For most individuals, non-surgical treatments are sufficient to manage symptoms and improve quality of life. These options include:
Physical Therapy
Physical therapy is one of the most effective ways to address degenerative disc disease. A trained therapist can design a personalized exercise program to strengthen the muscles supporting the spine, improve flexibility, and reduce pain. Common exercises include:
- Stretching routines to enhance mobility.
- Core strengthening exercises to stabilize the spine.
- Low-impact aerobic activities, such as swimming or walking.
Medications
Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can help alleviate mild to moderate pain. In more severe cases, a doctor may prescribe stronger medications, such as muscle relaxants or anti-inflammatory drugs.
Epidural Steroid Injections
These injections deliver anti-inflammatory medication directly to the affected area, providing temporary relief from pain and inflammation. They are often used when oral medications are insufficient.
Lifestyle Modifications
Making certain lifestyle changes can significantly reduce symptoms and slow the progression of degenerative disc disease. Examples include:
- Maintaining a healthy weight to reduce strain on the spine.
- Quitting smoking to improve blood flow to the discs.
- Practicing good posture to minimize stress on the spine.
Surgical Treatments
In cases where non-surgical treatments fail to provide relief, surgery may be considered. Surgical options are typically reserved for individuals with severe symptoms or significant nerve compression. Common procedures include:
Discectomy
A discectomy involves removing part or all of a damaged disc to relieve pressure on the nerves. This procedure is often performed using minimally invasive techniques, resulting in faster recovery times.
Spinal Fusion
Spinal fusion involves joining two or more vertebrae together to stabilize the spine and eliminate motion at the affected level. While effective, this procedure can limit flexibility and may lead to increased stress on adjacent discs.
Artificial Disc Replacement
This innovative procedure involves replacing a damaged disc with an artificial one. Unlike spinal fusion, artificial disc replacement preserves motion in the spine and may reduce the risk of future complications.
Preventive Measures
While degenerative disc disease cannot always be prevented, certain measures can help reduce the risk of developing severe symptoms. These include:
- Engaging in regular physical activity to maintain spinal health.
- Using proper lifting techniques to avoid straining the back.
- Incorporating ergonomic principles into daily activities, such as sitting and working at a desk.
- Seeking prompt medical attention for any spinal injuries or persistent pain.
The Role of Nutrition
A balanced diet rich in vitamins and minerals can support overall spinal health. Key nutrients include:
- Calcium: Essential for maintaining strong bones.
- Vitamin D: Helps the body absorb calcium and supports bone health.
- Omega-3 Fatty Acids: Found in fish and flaxseed, these can help reduce inflammation.
Mental Health Considerations
Chronic pain associated with degenerative disc disease can take a toll on mental health. It is important to address emotional well-being through:
- Stress management techniques, such as meditation or yoga.
- Seeking support from friends, family, or support groups.
- Consulting a mental health professional if needed.