A cystocele, also known as anterior vaginal wall prolapse or bladder prolapse, is a condition that occurs when the supportive tissues between a woman’s bladder and vaginal wall weaken. This weakening allows the bladder to bulge into the vagina, leading to various physical symptoms and discomfort. Often abbreviated as “CP,” this condition is more common in women who have experienced childbirth, menopause, or other factors that affect pelvic floor strength. In this article, we will explore the causes, symptoms, and treatment options for bladder prolapse in detail.
Understanding Bladder Prolapse
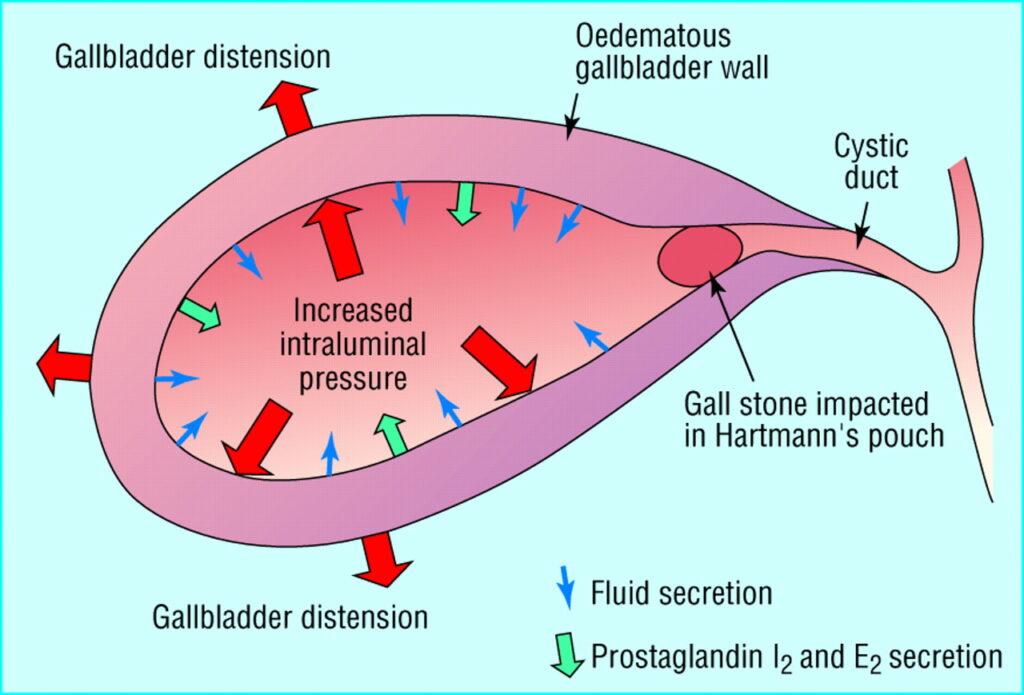
Bladder prolapse occurs when the muscles and connective tissues that support the bladder lose their strength. These tissues are part of the pelvic floor, a network of muscles and ligaments that hold the pelvic organs in place. When these structures weaken, the bladder can drop from its normal position and press against the front wall of the vagina. The severity of bladder prolapse varies, ranging from mild cases where the bulge is barely noticeable to severe cases where the bladder significantly protrudes into the vaginal canal.
Different Grades of Severity
- Mild: The bladder slightly drops but does not cause significant symptoms or discomfort.
- Moderate: The bladder descends further, causing noticeable bulging and discomfort.
- Severe: The bladder protrudes significantly into the vagina, often affecting daily activities and quality of life.
Causes of Bladder Prolapse
Several factors contribute to the weakening of pelvic floor muscles and connective tissues, leading to bladder prolapse. Understanding these causes can help individuals take preventive measures and seek appropriate treatment.
Childbirth
Vaginal childbirth is one of the most common causes of bladder prolapse. During delivery, the pelvic floor muscles and tissues are stretched and may sustain damage. Multiple pregnancies or difficult deliveries can increase the risk of developing this condition later in life.
Aging and Menopause
As women age, their bodies naturally produce less estrogen, a hormone that helps maintain the strength and elasticity of pelvic tissues. The decline in estrogen levels during menopause can weaken these tissues, making them more susceptible to prolapse.
Chronic Straining
Activities that involve chronic straining, such as heavy lifting, persistent coughing, or constipation, can put excessive pressure on the pelvic floor. Over time, this pressure can lead to the weakening of supportive tissues and result in bladder prolapse.
Obesity
Excess body weight places additional strain on the pelvic floor muscles. Women who are overweight or obese are at a higher risk of developing bladder prolapse due to the constant pressure exerted on the pelvic region.
Prior Pelvic Surgery
Surgical procedures involving the pelvic area, such as hysterectomy, can sometimes disrupt the supportive structures of the pelvis. This disruption may increase the likelihood of bladder prolapse occurring afterward.
Symptoms of Bladder Prolapse
The symptoms of bladder prolapse vary depending on the severity of the condition. Some women may experience mild discomfort, while others may face more pronounced symptoms that interfere with their daily lives.
Common Signs and Symptoms
- Sensation of Fullness or Pressure: Many women describe feeling a sense of fullness or pressure in the pelvic area, especially after standing for long periods or lifting heavy objects.
- Bulging Tissue: A visible or palpable bulge in the vagina is a hallmark symptom of bladder prolapse. This bulge may become more prominent when coughing, sneezing, or bearing down.
- Urinary Problems: Bladder prolapse can lead to urinary issues, including difficulty emptying the bladder completely, frequent urination, or stress incontinence (leakage of urine during physical activity).
- Pain or Discomfort: Women with bladder prolapse may experience discomfort during sexual intercourse or while performing everyday activities.
- Lower Back Pain: Some individuals report lower back pain, which may worsen as the day progresses.
Diagnosis of Bladder Prolapse
If you suspect you have bladder prolapse, it is essential to consult a healthcare provider for an accurate diagnosis. The diagnostic process typically involves a combination of medical history review, physical examination, and specialized tests.
Medical History and Physical Examination
Your doctor will begin by asking about your symptoms, medical history, and any factors that may have contributed to the condition. A thorough pelvic examination is then performed to assess the extent of the prolapse and determine its severity.
Additional Tests
- Urinary Function Tests: These tests evaluate how well the bladder is functioning and whether there are any underlying issues, such as urinary retention or incontinence.
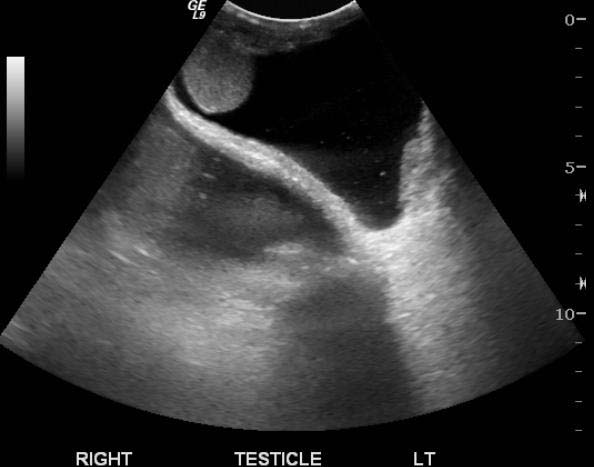
- Imaging Studies: In some cases, imaging techniques like ultrasound or magnetic resonance imaging may be used to get a clearer picture of the pelvic anatomy.
Treatment Options for Bladder Prolapse
Treatment for bladder prolapse depends on the severity of the condition, the presence of symptoms, and the individual’s overall health and preferences. There are both non-surgical and surgical options available to manage this condition effectively.
Non-Surgical Treatments
For mild to moderate cases of bladder prolapse, non-surgical treatments are often recommended as the first line of management.
Pelvic Floor Exercises
Also known as Kegel exercises, these involve contracting and relaxing the pelvic floor muscles to strengthen them. Regular practice can improve muscle tone and provide better support for the bladder.
Lifestyle Modifications
- Weight Management: Losing excess weight can reduce pressure on the pelvic floor and alleviate symptoms.
- Avoiding Heavy Lifting: Minimizing activities that strain the pelvic muscles can prevent further weakening.
- Treating Chronic Cough: Addressing underlying conditions like asthma or smoking-related coughs can reduce strain on the pelvic region.
Pessary Devices
A pessary is a removable device inserted into the vagina to support the bladder and hold it in place. It is a non-invasive option that can provide relief for women who are not candidates for surgery or prefer a temporary solution.
Surgical Treatments
In cases of severe bladder prolapse or when non-surgical methods fail to provide adequate relief, surgery may be recommended.
Anterior Vaginal Repair
This procedure involves reinforcing the weakened tissues between the bladder and the vagina using stitches. The goal is to restore the bladder to its normal position and alleviate symptoms.
Mesh Implants
In some cases, synthetic mesh may be used to provide additional support to the pelvic floor. However, the use of mesh implants has been associated with complications, so this option requires careful consideration and discussion with a healthcare provider.
Hysterectomy
If bladder prolapse is accompanied by uterine prolapse, a hysterectomy (removal of the uterus) may be performed as part of the treatment plan. This procedure can address multiple pelvic organ prolapses simultaneously.
Preventing Bladder Prolapse
While not all cases of bladder prolapse can be prevented, certain measures can reduce the risk of developing this condition or minimize its progression.
Maintaining a Healthy Weight
Staying within a healthy weight range reduces the strain on the pelvic floor muscles and lowers the risk of prolapse.
Performing Regular Pelvic Floor Exercises
Consistently practicing pelvic floor exercises can help maintain muscle strength and prevent weakening over time.
Avoiding Excessive Strain
Limiting activities that place undue pressure on the pelvic region, such as heavy lifting or chronic coughing, can protect the supportive tissues.
Seeking Timely Medical Care
Addressing symptoms early and seeking medical advice promptly can prevent the condition from worsening and improve outcomes.