Cryptorchidism, commonly referred to as undescended testicle, is a condition that affects male infants and is characterized by the failure of one or both testicles to descend into the scrotum before birth. This condition is one of the most common congenital anomalies in newborn boys and requires timely medical attention to prevent potential complications. In this article, we will explore the overview, causes, diagnosis, and treatment options for undescended testicles.
What is an Undescended Testicle?
An undescended testicle occurs when one or both testicles fail to move into their proper position in the scrotum during fetal development. Normally, the testicles develop inside the abdomen and gradually descend into the scrotum during the last few months of pregnancy. When this process does not occur as expected, it results in cryptorchidism.
This condition is typically identified shortly after birth during routine physical examinations. It is more common in premature infants but can also occur in full-term babies. If left untreated, an undescended testicle can lead to complications such as infertility, increased risk of testicular cancer, and hernias.
Causes of Undescended Testicles
The exact cause of undescended testicles is not always clear, but several factors may contribute to its development:
Hormonal Factors
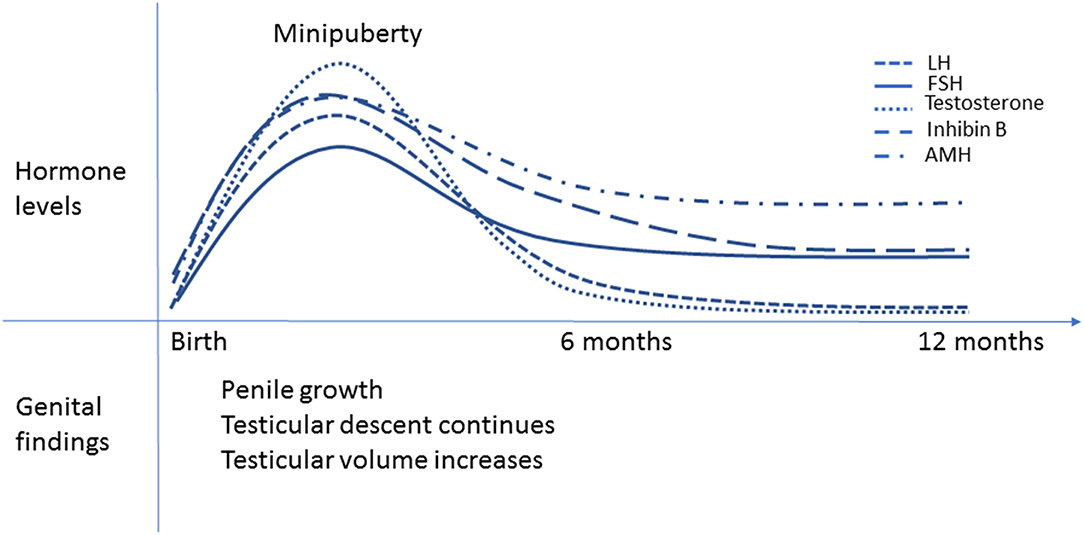
- Inadequate Hormone Production: The descent of the testicles is influenced by hormones such as testosterone. If the fetus does not produce sufficient levels of these hormones, it may result in incomplete descent.
- Maternal Health: Certain maternal health conditions, such as diabetes or obesity, have been linked to an increased risk of undescended testicles in newborns.
Genetic Factors
- Family History: A family history of undescended testicles or other genital abnormalities may increase the likelihood of the condition occurring in future generations.
- Chromosomal Abnormalities: Some genetic syndromes, such as Klinefelter syndrome or Down syndrome, are associated with a higher incidence of undescended testicles.
Environmental Factors
- Prenatal Exposure to Toxins: Exposure to certain environmental toxins, such as pesticides or chemicals, during pregnancy may interfere with normal fetal development.
- Smoking and Alcohol Use: Maternal smoking or excessive alcohol consumption during pregnancy has been linked to an increased risk of undescended testicles.
Symptoms of Undescended Testicles
In most cases, undescended testicles do not cause noticeable symptoms beyond the absence of one or both testicles in the scrotum. However, parents or caregivers may notice the following signs:
- An empty or underdeveloped scrotum on one or both sides
- A small lump in the groin area that may represent the undescended testicle
- Absence of testicles in the scrotum during diaper changes or bathing
It is important to note that some infants may have retractile testicles, a condition where the testicles temporarily move out of the scrotum due to muscle contractions. This is different from true undescended testicles and usually resolves on its own.
Diagnosis of Undescended Testicles
Diagnosing undescended testicles typically involves a combination of physical examinations and imaging tests. Early detection is crucial to ensure appropriate treatment and prevent complications.
Physical Examination
A healthcare provider will perform a thorough physical examination of the infant’s genital area. During this exam, the doctor will gently feel the scrotum and groin region to locate the testicles. In some cases, the testicle may be felt in the inguinal canal, which is the passage through which it should have descended.
Imaging Tests
If the testicle cannot be located during the physical examination, additional imaging tests may be required:
- Ultrasound: An ultrasound of the scrotum and groin area can help identify the location of the undescended testicle.
- Magnetic Resonance Imaging (MRI): In rare cases, an MRI may be used to provide detailed images of the pelvic region.
Differential Diagnosis
It is important to differentiate undescended testicles from other conditions that may present similar symptoms, such as retractile testicles or absent testicles. A careful evaluation by a pediatrician or urologist is essential to make an accurate diagnosis.
Treatment Options for Undescended Testicles
Treatment for undescended testicles aims to ensure that the testicles are positioned correctly in the scrotum to promote normal development and function. The choice of treatment depends on the age of the child, the location of the testicle, and the severity of the condition.
Observation and Monitoring
In some cases, undescended testicles may descend on their own within the first few months of life. For this reason, healthcare providers often recommend a period of observation before pursuing intervention. Regular follow-up appointments are scheduled to monitor the progress of the testicle’s descent.
Hormonal Therapy
Hormonal therapy involves the use of medications, such as human chorionic gonadotropin (HCG), to stimulate the descent of the testicle. This treatment is typically considered for infants whose testicles are close to descending but have not yet reached the scrotum. While hormonal therapy can be effective in some cases, it is not always successful and may require additional interventions.
Surgical Intervention
Surgery, known as orchiopexy, is the most common and effective treatment for undescended testicles. This procedure involves making a small incision in the groin area to locate the undescended testicle and repositioning it into the scrotum. Orchiopexy is typically performed on an outpatient basis and is most effective when done between six months and one year of age.
Benefits of surgical intervention include:
- Reduced risk of infertility
- Lower likelihood of developing testicular cancer
- Improved cosmetic appearance of the scrotum
Post-Surgical Care
After surgery, the child will need to follow specific care instructions to ensure proper healing. These may include:
- Avoiding strenuous activities for a few weeks
- Keeping the surgical site clean and dry
- Attending follow-up appointments to monitor recovery
Potential Complications of Untreated Undescended Testicles
If left untreated, undescended testicles can lead to several complications, including:
- Infertility: Testicles that remain undescended may not develop properly, leading to reduced sperm production and fertility issues later in life.
- Testicular Cancer: Men with a history of undescended testicles have a higher risk of developing testicular cancer, even if the condition was corrected surgically.
- Hernias: Undescended testicles are often associated with inguinal hernias, which occur when part of the intestine protrudes through a weak spot in the abdominal muscles.
- Torsion: The undescended testicle is at risk of twisting, which can cut off its blood supply and cause severe pain and damage.
Preventive Measures and Parental Guidance
While undescended testicles cannot always be prevented, there are steps parents can take to reduce the risk and ensure early detection:
- Prenatal Care: Regular prenatal check-ups and maintaining a healthy lifestyle during pregnancy can help minimize the risk of complications.
- Routine Examinations: Parents should regularly check their child’s genital area for any abnormalities and report concerns to a healthcare provider.
- Educating Caregivers: Informing babysitters, daycare providers, and other caregivers about the condition can ensure consistent monitoring and prompt reporting of any changes.
When to Seek Medical Attention
Parents should seek medical attention if they notice any of the following:
- Absence of one or both testicles in the scrotum after six months of age
- Swelling, redness, or pain in the groin or scrotum
- Changes in the size or shape of the scrotum
Early intervention is key to addressing undescended testicles and minimizing the risk of long-term complications.