Crohn’s disease, often abbreviated as CD, is a chronic inflammatory condition that primarily affects the digestive tract. This condition belongs to a group of disorders known as inflammatory bowel diseases and can have a significant impact on a person’s quality of life. Understanding its causes, recognizing its symptoms, and exploring available treatments are crucial steps in managing this challenging condition.
What Is Crohn’s Disease?
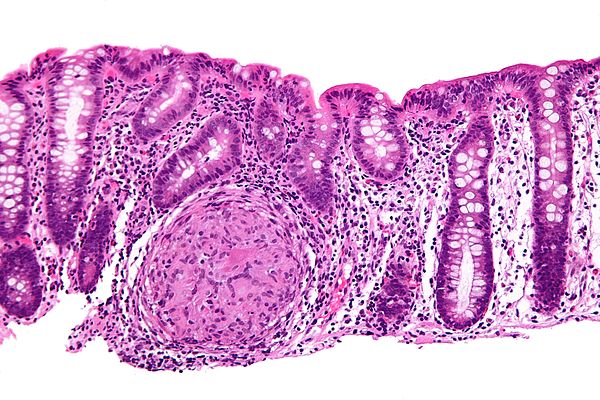
Crohn’s disease is a type of inflammatory bowel disease that can affect any part of the gastrointestinal tract, from the mouth to the anus. However, it most commonly impacts the end of the small intestine, known as the ileum, and the beginning of the large intestine, or colon. Unlike some other digestive disorders, Crohn’s disease can penetrate deep into the layers of the affected bowel tissue, leading to severe complications if left untreated.
The hallmark of this condition is inflammation, which can occur in patches, leaving areas of healthy tissue interspersed with inflamed regions. This characteristic makes it distinct from ulcerative colitis, another form of inflammatory bowel disease that typically affects only the innermost lining of the colon and rectum.
Key Features of Crohn’s Disease
- Chronic inflammation of the gastrointestinal tract
- Patchy distribution of affected areas
- Potential to involve all layers of the intestinal wall
- Unpredictable flare-ups and periods of remission
Causes of Crohn’s Disease
The exact cause of Crohn’s disease remains unknown, but researchers believe it results from a combination of genetic, environmental, and immune system factors. While no single factor has been identified as the sole cause, several contributing elements have been recognized.
Genetic Factors
Family history plays a significant role in the development of this condition. Individuals who have a close relative, such as a parent or sibling, with Crohn’s disease are at a higher risk of developing it themselves. Studies have identified specific genes that may increase susceptibility, suggesting a hereditary component to the disease.
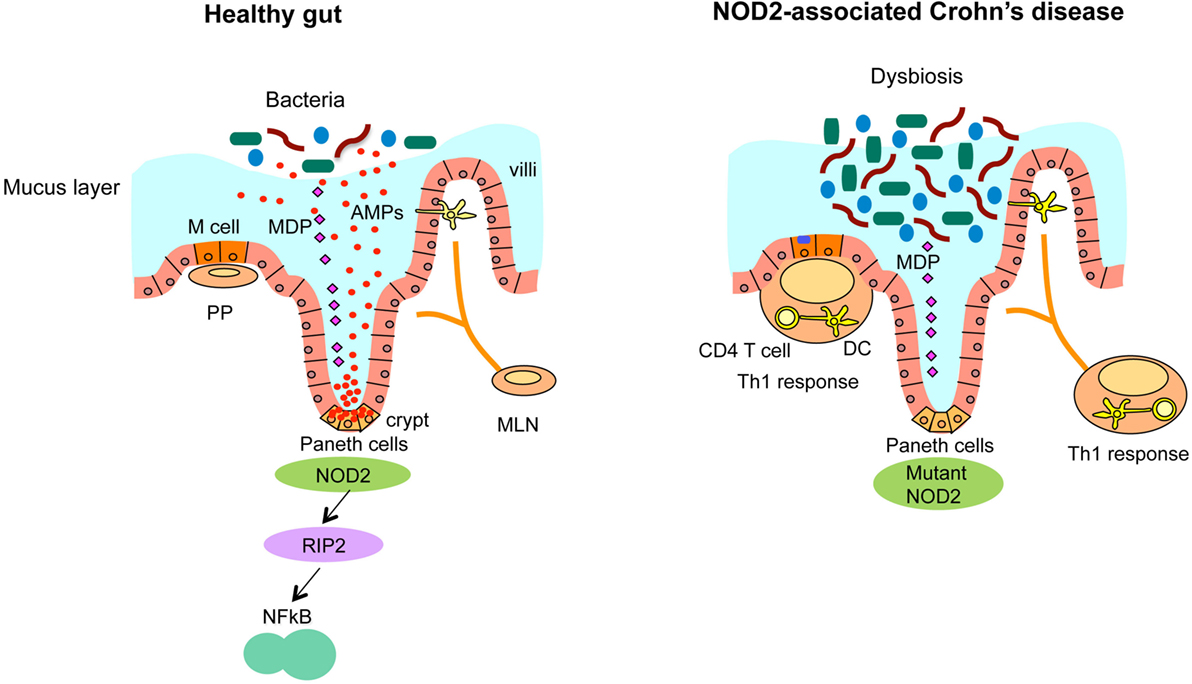
Immune System Dysfunction
Crohn’s disease is thought to arise when the immune system mistakenly attacks healthy cells in the gastrointestinal tract. Normally, the immune system defends the body against harmful invaders like bacteria and viruses. In people with this condition, however, the immune response becomes overactive and targets the digestive tract, causing inflammation and damage.
Environmental Triggers
Several environmental factors have been linked to an increased risk of developing this condition. These include smoking, a diet high in fat or refined foods, and living in urban or industrialized areas. Additionally, certain infections and the use of nonsteroidal anti-inflammatory medications may exacerbate or trigger symptoms in susceptible individuals.
Microbiome Imbalance
The gut microbiome, which consists of trillions of microorganisms living in the digestive tract, plays a vital role in maintaining health. An imbalance in these microorganisms, often referred to as dysbiosis, has been observed in individuals with Crohn’s disease. This imbalance may contribute to inflammation and worsen symptoms.
Symptoms of Crohn’s Disease
The symptoms of Crohn’s disease can vary widely depending on the location and severity of inflammation. Some individuals experience mild symptoms, while others may face debilitating complications. The condition is also characterized by periods of flare-ups, where symptoms worsen, and remission, where they subside.
Gastrointestinal Symptoms
The most common symptoms of this condition are related to the digestive system. These include:
- Abdominal pain and cramping
- Diarrhea, which may be persistent or intermittent
- Blood in the stool
- Urgent need to have a bowel movement
- Nausea and vomiting
Systemic Symptoms
In addition to digestive issues, Crohn’s disease can cause symptoms that affect the entire body. These systemic symptoms include:
- Fatigue and weakness
- Unintended weight loss
- Fever and night sweats
- Loss of appetite
Complications and Extraintestinal Manifestations
Crohn’s disease can lead to complications both within and outside the digestive tract. Some potential complications include:
- Bowel obstructions caused by scarring and narrowing of the intestines
- Fistulas, or abnormal connections between different parts of the intestines or other organs
- Ulcers in the mouth, stomach, or intestines
- Nutritional deficiencies due to malabsorption of nutrients
Extraintestinal manifestations, or symptoms affecting other parts of the body, are also common. These may include joint pain, skin rashes, eye inflammation, and liver disorders.
Treatments for Crohn’s Disease
While there is currently no cure for this condition, various treatment options are available to manage symptoms, reduce inflammation, and improve quality of life. Treatment plans are highly individualized and depend on the severity of the disease, the location of inflammation, and the patient’s overall health.
Medications
Medications are often the first line of treatment for managing this condition. These drugs aim to control inflammation, suppress the immune system, and alleviate symptoms. Commonly prescribed medications include:
- Aminosalicylates, which help reduce inflammation in mild to moderate cases
- Corticosteroids, used for short-term control of severe flare-ups
- Immunomodulators, which suppress the immune system to prevent ongoing inflammation
- Biologic therapies, which target specific proteins involved in the inflammatory process
Dietary and Lifestyle Changes
Making adjustments to diet and lifestyle can play a significant role in managing symptoms. While no specific diet has been proven to cure this condition, certain dietary changes may help reduce discomfort and improve overall well-being. These include:
- Eating smaller, more frequent meals to ease digestion
- Avoiding trigger foods, such as those high in fiber, fat, or spice
- Staying hydrated to prevent dehydration caused by diarrhea
- Taking nutritional supplements to address deficiencies
Lifestyle modifications, such as quitting smoking, exercising regularly, and managing stress, can also support better health outcomes.
Surgery
In cases where medication and lifestyle changes are insufficient, surgery may be necessary. Surgery is not a cure but can help address complications and improve symptoms. Common surgical procedures include:
- Removal of damaged portions of the intestines
- Repair of fistulas or abscesses
- Widening of narrowed areas in the intestines
It is important to note that surgery does not eliminate the risk of future flare-ups, as inflammation can recur in other parts of the digestive tract.
Emerging Therapies
Research into new treatments for this condition is ongoing, with promising developments on the horizon. Emerging therapies include:
- Stem cell transplantation to reset the immune system
- Microbiome-based treatments aimed at restoring balance to gut bacteria
- Targeted therapies designed to block specific pathways involved in inflammation
These innovative approaches hold the potential to revolutionize the management of this condition in the future.
Living with Crohn’s Disease
Managing this condition requires a comprehensive approach that addresses both physical and emotional well-being. Support from healthcare providers, family, and peers can make a significant difference in coping with the challenges of this condition. Joining support groups, seeking counseling, and staying informed about the latest advancements in treatment can empower individuals to take control of their health.
Tips for Managing Daily Life
- Work closely with a healthcare team to develop a personalized treatment plan
- Keep a symptom diary to identify triggers and track progress
- Prioritize self-care and stress management techniques
- Educate friends and family about the condition to foster understanding and support