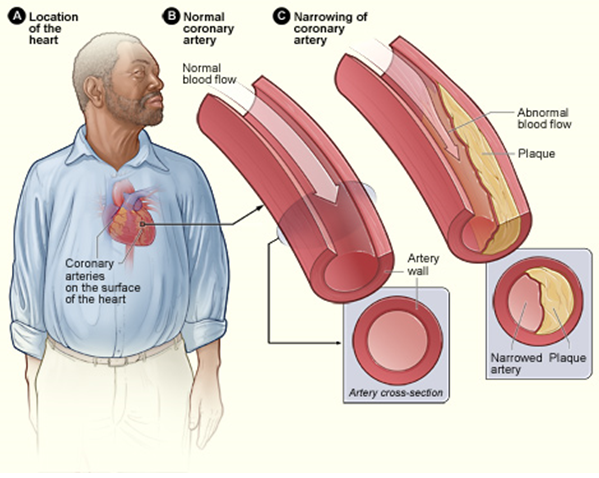
Coronary artery disease, often abbreviated as CAD, is one of the most common forms of heart disease and a leading cause of death worldwide. It occurs when the arteries that supply blood to the heart muscle become narrowed or blocked due to the buildup of fatty deposits, cholesterol, and other substances. This condition can lead to serious complications, including heart attacks, if left untreated. Understanding coronary artery disease, its risk factors, symptoms, and care strategies is essential for prevention and effective management.
What is Coronary Artery Disease?
Coronary artery disease develops when the coronary arteries, which are responsible for delivering oxygen-rich blood to the heart, become damaged or diseased. The primary cause of this damage is atherosclerosis, a process in which plaque builds up on the inner walls of the arteries. Plaque is made up of fat, cholesterol, calcium, and other substances found in the blood. Over time, this buildup can harden and narrow the arteries, restricting blood flow to the heart muscle.
When the heart does not receive enough oxygen-rich blood, it can lead to chest pain, shortness of breath, and other symptoms. In severe cases, a complete blockage of an artery can result in a heart attack, which occurs when part of the heart muscle is deprived of oxygen and begins to die.
How Does Coronary Artery Disease Develop?
The development of coronary artery disease is a gradual process that often begins in early adulthood. Several factors contribute to the formation of plaque in the arteries:
- High levels of cholesterol: Excess cholesterol in the blood can stick to the walls of the arteries, forming plaque.
- High blood pressure: Increased pressure in the arteries can damage their inner lining, making it easier for plaque to build up.
- Smoking: Tobacco smoke contains chemicals that can irritate the lining of the arteries and promote plaque formation.
- Inflammation: Chronic inflammation in the body can contribute to the development of atherosclerosis.
As plaque accumulates, it can cause the arteries to narrow, reducing blood flow to the heart. In some cases, a piece of plaque may break off, forming a blood clot that further obstructs blood flow and increases the risk of a heart attack.
Risk Factors for Coronary Artery Disease
Several factors increase the likelihood of developing coronary artery disease. While some of these factors are beyond an individual’s control, others can be managed through lifestyle changes and medical interventions.
Non-Modifiable Risk Factors
These are factors that cannot be changed but play a significant role in the development of coronary artery disease:
- Age: The risk of coronary artery disease increases with age. Men over the age of 45 and women over the age of 55 are at higher risk.
- Family history: A family history of heart disease, especially if a close relative developed it at an early age, increases the risk.
- Gender: Men are generally at higher risk than women, although the risk for women increases after menopause.
Modifiable Risk Factors
These are factors that can be controlled or managed to reduce the risk of coronary artery disease:
- Unhealthy diet: Consuming foods high in saturated fats, trans fats, cholesterol, and sodium can contribute to plaque buildup in the arteries.
- Lack of physical activity: A sedentary lifestyle can lead to obesity, high blood pressure, and other conditions that increase the risk of heart disease.
- Smoking: Smoking damages the lining of the arteries and reduces the amount of oxygen in the blood, making the heart work harder.
- Obesity: Excess body weight is associated with high blood pressure, high cholesterol, and diabetes, all of which are risk factors for coronary artery disease.
- Diabetes: High blood sugar levels can damage blood vessels and contribute to the development of atherosclerosis.
- Stress: Chronic stress can raise blood pressure and contribute to unhealthy habits such as smoking or overeating.
Symptoms of Coronary Artery Disease
The symptoms of coronary artery disease vary depending on the severity of the condition and the individual. Some people may experience no symptoms at all, while others may have mild to severe symptoms. Common signs and symptoms include:
Chest Pain (Angina)
Chest pain, also known as angina, is one of the most common symptoms of coronary artery disease. It typically feels like pressure, tightness, or squeezing in the chest and may radiate to the shoulders, arms, neck, jaw, or back. Angina often occurs during physical activity or emotional stress and may improve with rest or medication.
Shortness of Breath
Shortness of breath can occur when the heart is unable to pump enough blood to meet the body’s needs. This symptom may be accompanied by fatigue, dizziness, or lightheadedness.
Heart Attack
A heart attack is a serious complication of coronary artery disease and requires immediate medical attention. Symptoms of a heart attack include:
- Chest pain or discomfort that lasts more than a few minutes or goes away and comes back
- Pain or discomfort in the arms, back, neck, jaw, or stomach
- Shortness of breath
- Nausea, vomiting, or lightheadedness
It is important to note that some individuals, particularly women, older adults, and people with diabetes, may experience atypical symptoms or no symptoms at all before a heart attack.
Diagnosis and Treatment of Coronary Artery Disease
Early diagnosis and treatment are crucial for managing coronary artery disease and preventing complications. Healthcare providers use a combination of tests and procedures to diagnose the condition and develop a personalized treatment plan.
Diagnostic Tests
Several tests are used to diagnose coronary artery disease:
- Electrocardiogram (ECG): This test records the electrical activity of the heart and can detect irregularities in heart rhythm or evidence of a previous heart attack.
- Stress test: During a stress test, the patient exercises on a treadmill or stationary bike while their heart rate, blood pressure, and ECG are monitored.
- Coronary angiography: This imaging test uses dye and X-rays to visualize the inside of the coronary arteries and identify blockages.
- Blood tests: Blood tests can measure cholesterol levels, blood sugar levels, and other markers of heart health.
Treatment Options
Treatment for coronary artery disease focuses on relieving symptoms, improving blood flow to the heart, and reducing the risk of complications. Treatment options include:
- Lifestyle changes: Adopting a healthy diet, exercising regularly, quitting smoking, and managing stress can significantly improve heart health.
- Medications: Medications such as aspirin, beta-blockers, statins, and ACE inhibitors may be prescribed to manage symptoms and reduce the risk of heart attack.
- Medical procedures: Procedures such as angioplasty and stent placement or coronary artery bypass surgery may be recommended to restore blood flow to the heart.
Prevention and Care Strategies
Preventing coronary artery disease involves adopting a heart-healthy lifestyle and addressing modifiable risk factors. Here are some key strategies for prevention and care:
Eat a Heart-Healthy Diet
A diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can help lower cholesterol levels, reduce blood pressure, and maintain a healthy weight. Limiting the intake of processed foods, sugary beverages, and foods high in saturated and trans fats is also important.
Stay Physically Active
Regular physical activity strengthens the heart, improves circulation, and helps maintain a healthy weight. Aim for at least 150 minutes of moderate-intensity exercise or 75 minutes of vigorous-intensity exercise each week.
Quit Smoking
Quitting smoking is one of the most effective ways to reduce the risk of coronary artery disease. Nicotine replacement therapy, counseling, and support groups can help individuals quit successfully.
Manage Stress
Chronic stress can negatively impact heart health. Practicing relaxation techniques such as deep breathing, meditation, or yoga can help reduce stress levels.
Monitor and Control Health Conditions
Managing conditions such as high blood pressure, high cholesterol, and diabetes is essential for preventing coronary artery disease. Regular check-ups with a healthcare provider can help monitor these conditions and adjust treatment plans as needed.
Living with Coronary Artery Disease
For individuals diagnosed with coronary artery disease, living a full and active life is possible with proper care and management. Adhering to a treatment plan, staying informed about the condition, and seeking support from healthcare professionals and loved ones can make a significant difference.
Support groups and educational resources are available to help individuals and their families cope with the challenges of living with coronary artery disease. By taking proactive steps and working closely with healthcare providers, it is possible to minimize symptoms, prevent complications, and improve overall quality of life.