Complex Regional Pain Syndrome, often abbreviated as CRPS, is a chronic and debilitating condition that affects millions of people worldwide. This disorder primarily impacts the limbs, causing intense pain and other symptoms that can significantly disrupt daily life. While the exact cause of this condition remains unclear, understanding its mechanisms, recognizing its symptoms, and exploring available treatments are essential steps toward managing it effectively.
What is Complex Regional Pain Syndrome?
Complex Regional Pain Syndrome is a rare neurological disorder characterized by severe, persistent pain that typically affects one limb, such as an arm, leg, hand, or foot. The condition usually develops after an injury, surgery, stroke, or heart attack but can also occur without any apparent triggering event. It is believed to arise from dysfunction in the central and peripheral nervous systems, leading to abnormal responses in how the body perceives pain.
There are two main types of this syndrome:
- Type 1: This form occurs after an injury or illness that did not directly damage the nerves in the affected limb. It was previously referred to as reflex sympathetic dystrophy.
- Type 2: This type arises from a distinct nerve injury and was formerly known as causalgia.
Both types share similar symptoms, though the underlying causes may differ slightly. Regardless of the type, the condition is marked by disproportionate levels of pain compared to the initial injury or event.
Symptoms of Complex Regional Pain Syndrome
The symptoms of this condition can vary widely among individuals, but they generally include a combination of physical, sensory, and emotional manifestations. These symptoms often progress over time and can become more severe if left untreated.
Pain and Sensitivity
The hallmark symptom of this condition is intense, continuous pain that feels out of proportion to the initial injury. This pain is often described as burning, throbbing, or stabbing and may worsen with even the slightest touch or movement. Some individuals report heightened sensitivity to stimuli such as temperature changes, pressure, or vibrations, making everyday activities challenging.
Swelling and Changes in Skin Appearance
In addition to pain, swelling is a common early symptom. The affected limb may appear swollen, tender, and warm to the touch. Over time, changes in skin texture and color may occur. For example, the skin might become shiny, thin, or discolored, ranging from pale to red or purple. These changes are often accompanied by excessive sweating in the affected area.
Muscle and Joint Problems
Individuals with this condition frequently experience muscle weakness, stiffness, and spasms. Joints in the affected limb may become stiff, limiting mobility and making it difficult to perform routine tasks. In severe cases, muscle atrophy (wasting) can occur due to prolonged disuse of the limb.
Other Symptoms
Beyond the primary symptoms, some individuals may notice additional issues, including:
- Hair and nail growth changes in the affected limb
- Difficulty moving the limb due to pain or stiffness
- Emotional challenges such as anxiety, depression, or irritability stemming from chronic pain
These symptoms can fluctuate in intensity and may spread to other parts of the body in rare cases. Early recognition and intervention are crucial for preventing the progression of the condition.
Causes and Risk Factors
The exact cause of this syndrome remains poorly understood, but researchers believe it involves a combination of factors related to the nervous system, immune response, and genetic predisposition. Several potential triggers have been identified, including:
- Trauma or injury to a limb, such as fractures, sprains, or surgical procedures
- Stroke or heart attack
- Prolonged immobilization of a limb, such as wearing a cast
- Infections or inflammatory conditions
While anyone can develop this condition, certain factors may increase the risk. These include:
- Being female, as women are more commonly affected than men
- A history of previous injuries or surgeries
- Underlying health conditions such as migraines, osteoporosis, or autoimmune disorders
It is important to note that not everyone who experiences these risk factors will develop the condition, highlighting the complexity of its origins.
Diagnosing the Condition
Diagnosing this syndrome can be challenging because there is no single test to confirm its presence. Instead, healthcare providers rely on a combination of clinical evaluations, medical history, and diagnostic criteria to make an accurate diagnosis. One widely used set of guidelines is the Budapest Criteria, which outlines specific signs and symptoms that must be present for a diagnosis.
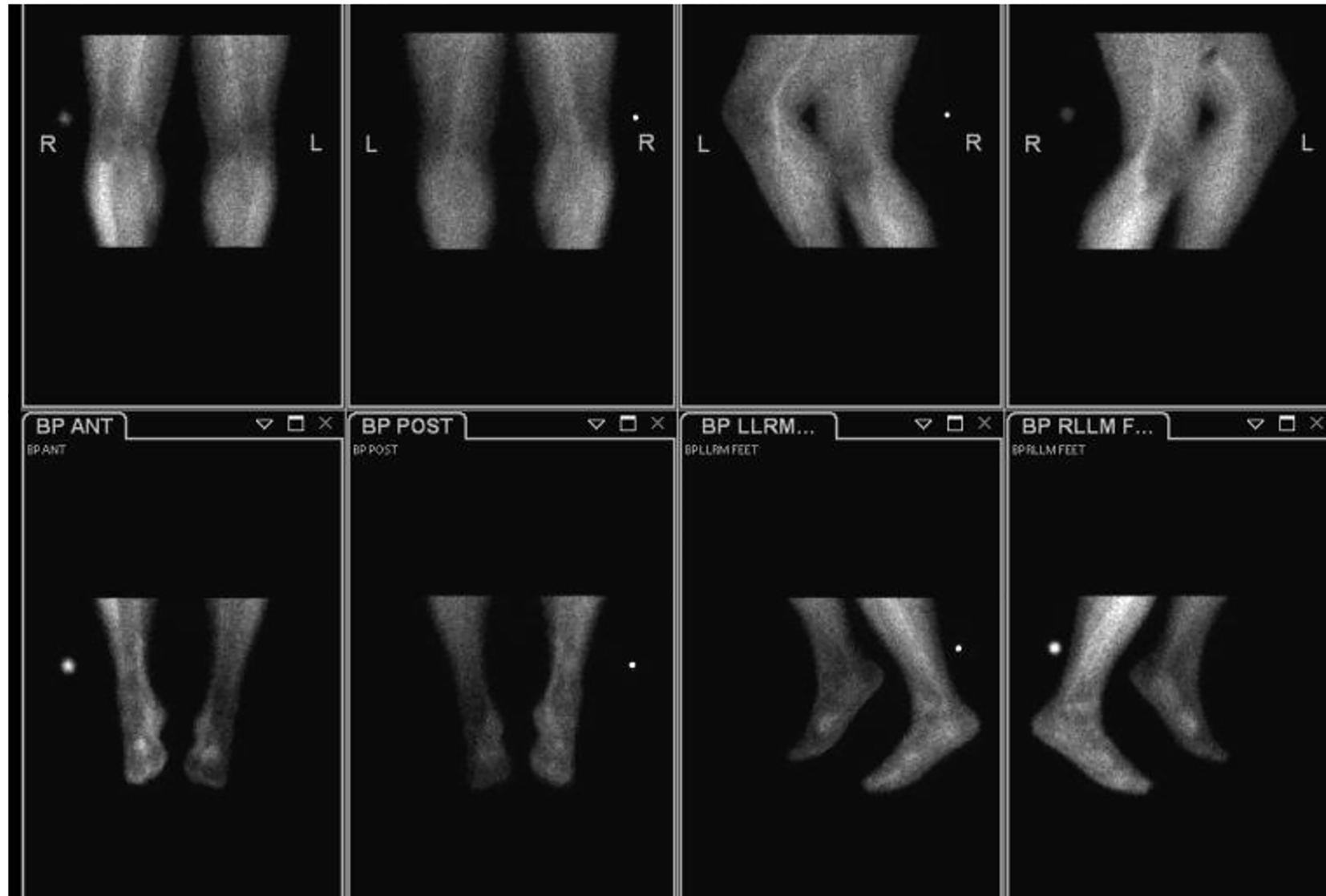
During the evaluation process, doctors may order imaging tests such as X-rays, bone scans, or magnetic resonance imaging to rule out other conditions and assess changes in bone density or tissue structure. Nerve conduction studies may also be performed to evaluate the function of the nerves in the affected limb.
Early diagnosis is critical, as prompt treatment can help prevent the condition from progressing and improve outcomes. However, delays in diagnosis are common due to the variability of symptoms and lack of awareness about the condition.
Treatment Options
While there is no cure for this condition, various treatments can help manage symptoms, improve function, and enhance quality of life. A multidisciplinary approach involving medical, physical, and psychological interventions is often recommended.
Medications
Several medications may be prescribed to alleviate pain and address other symptoms:
- Pain relievers: Over-the-counter or prescription pain medications, such as nonsteroidal anti-inflammatory drugs, may provide relief for mild cases.
- Nerve-blocking agents: Medications like lidocaine patches or nerve blocks can target specific areas of pain.
- Antidepressants and anticonvulsants: These drugs are sometimes used to treat nerve-related pain.
- Bisphosphonates: These medications may help reduce bone loss associated with the condition.
It is important to work closely with a healthcare provider to find the most effective medication regimen, as responses to treatment can vary.
Physical Therapy
Physical therapy plays a key role in managing this condition by improving strength, flexibility, and mobility in the affected limb. A customized exercise program can help prevent muscle atrophy and joint stiffness while promoting circulation. Techniques such as graded motor imagery and mirror therapy may also be incorporated to retrain the brain’s perception of pain.
Psychological Support
Living with chronic pain can take a toll on mental health, making psychological support an essential component of treatment. Cognitive-behavioral therapy, counseling, and support groups can help individuals cope with the emotional challenges of the condition and develop strategies for managing stress and anxiety.
Interventional Procedures
In some cases, interventional procedures may be recommended to address severe or refractory symptoms. These include:
- Spinal cord stimulation: This involves implanting a device that delivers electrical impulses to the spinal cord to block pain signals.
- Sympathetic nerve blocks: Injecting anesthetic agents near the affected nerves can temporarily relieve pain.
These procedures are typically considered when conservative treatments have not provided sufficient relief.
Lifestyle Modifications
Making certain lifestyle changes can also support overall well-being and symptom management. These may include:
- Practicing relaxation techniques such as deep breathing, meditation, or yoga
- Maintaining a balanced diet to support overall health
- Avoiding smoking and excessive alcohol consumption, which can exacerbate symptoms
Collaborating with a team of healthcare professionals, including physicians, physical therapists, and mental health specialists, can help create a comprehensive treatment plan tailored to individual needs.
Research and Future Directions
Ongoing research is shedding light on the underlying mechanisms of this condition and paving the way for new treatment options. Scientists are exploring the role of inflammation, immune system dysfunction, and genetic factors in the development of the syndrome. Advances in neuroimaging and biomarker identification may lead to earlier and more accurate diagnoses in the future.
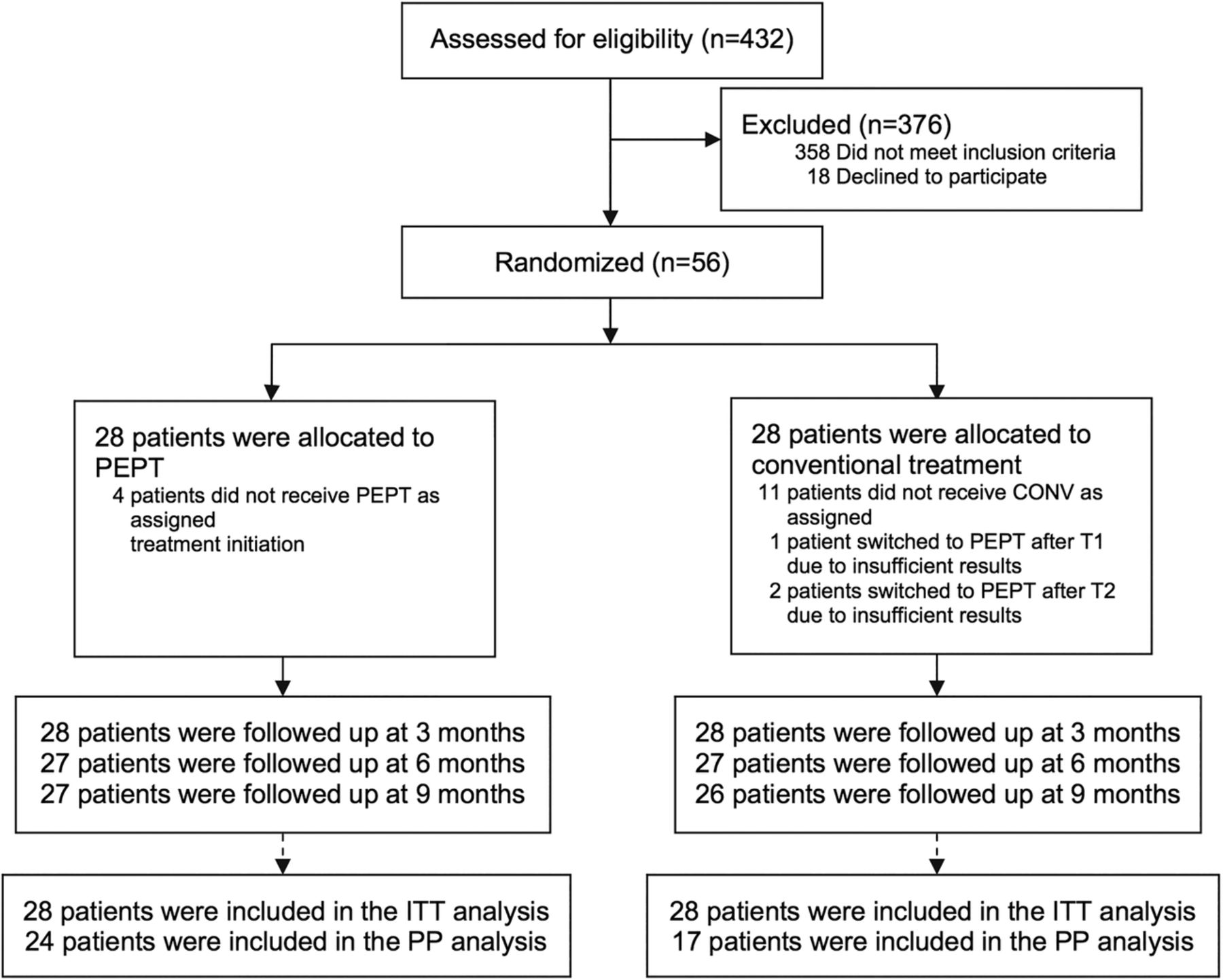
Emerging therapies, such as stem cell therapy and novel pharmacological agents, hold promise for addressing the root causes of the condition rather than merely alleviating symptoms. Clinical trials are underway to evaluate the safety and efficacy of these innovative approaches.
Raising awareness about this condition is also critical for ensuring timely diagnosis and access to care. Advocacy efforts by patient organizations and healthcare professionals are helping to educate the public and reduce stigma surrounding chronic pain conditions.