A coma is a profound state of unconsciousness where an individual is unable to respond to their surroundings or stimuli. This condition, often abbreviated as “coma,” can result from various medical conditions and injuries. In this article, we will explore the causes, symptoms, and recovery processes associated with this complex medical state.
What is a Coma?
A coma represents one of the most severe forms of altered consciousness. It is characterized by a deep state of unconsciousness in which the individual cannot be awakened, fails to respond normally to pain or light, and lacks voluntary actions. The person in a coma may appear to be asleep, but unlike sleep, they do not exhibit typical brain activity patterns associated with restorative rest.
Key Features of a Coma
- Unresponsiveness to external stimuli
- Lack of voluntary movements
- No evidence of awareness
- Irregular breathing and reflexes
Causes of a Coma
There are numerous potential causes for a coma, ranging from traumatic injuries to underlying health conditions. These causes can generally be grouped into three categories: traumatic brain injuries, metabolic or toxic conditions, and structural brain abnormalities.
Traumatic Brain Injuries
Traumatic brain injuries occur when an external force damages the brain. Common scenarios include car accidents, falls, sports injuries, and physical assaults. The severity of the injury determines whether the individual enters a coma. Severe trauma can cause swelling, bleeding, or direct damage to critical areas of the brain responsible for consciousness.
Metabolic or Toxic Conditions
Metabolic imbalances and exposure to toxins can also lead to a coma. Examples include:
- Diabetic emergencies: Extremely high or low blood sugar levels can impair brain function.
- Liver failure: When the liver cannot filter toxins, harmful substances accumulate in the bloodstream, affecting the brain.
- Kidney failure: Similar to liver failure, kidney dysfunction leads to toxin buildup.
- Poisoning: Overdose of drugs, alcohol, or other toxic substances can depress brain activity.
Structural Brain Abnormalities
Conditions that affect the structure of the brain can also result in a coma. These include:
- Stroke: A blockage or rupture of blood vessels in the brain can disrupt oxygen supply, leading to loss of consciousness.
- Tumors: Brain tumors can press on vital areas, interfering with normal brain function.
- Infections: Meningitis, encephalitis, or other infections of the central nervous system can cause inflammation and swelling, resulting in a coma.
Symptoms of a Coma
The primary symptom of a coma is the inability to regain consciousness. However, there are additional signs that healthcare providers look for when diagnosing this condition.
Physical Signs
- Closed eyes that do not open spontaneously
- No response to verbal commands or physical touch
- Abnormal breathing patterns
- Suppressed reflexes such as gagging or coughing
Neurological Indicators
Beyond physical signs, specific neurological assessments help determine the depth and nature of the coma. These include:
- Glasgow Coma Scale: A standardized tool used to assess the level of consciousness based on eye-opening, verbal responses, and motor reactions.
- Pupil reaction: Observing how the pupils respond to light provides insight into brainstem function.
- Muscle tone: Flaccidity or rigidity in muscles indicates varying degrees of brain impairment.
Diagnosis of a Coma
When someone enters a coma, immediate medical evaluation is crucial. Healthcare professionals employ a combination of clinical assessments and diagnostic tests to identify the underlying cause and plan appropriate treatment.
Clinical Assessment
The initial step involves gathering information about the circumstances surrounding the onset of the coma. This includes reviewing the patient’s medical history, recent illnesses, medications, and any incidents like accidents or seizures.
Diagnostic Tests
To pinpoint the exact cause, doctors rely on advanced imaging and laboratory tests:
- Computed Tomography (CT) Scan: Provides detailed images of the brain to detect bleeding, swelling, or structural abnormalities.
- Magnetic Resonance Imaging (MRI): Offers more precise visualization of soft tissues, useful for identifying subtle changes or lesions.
- Electroencephalogram (EEG): Measures electrical activity in the brain, helping differentiate between different states of unconsciousness.
- Blood Tests: Check for metabolic imbalances, infections, or drug toxicity.
Treatment Approaches
Treatment for a coma focuses on addressing the underlying cause while supporting vital functions. The approach varies depending on the specific condition responsible for the coma.
Immediate Interventions
In emergency situations, stabilizing the patient is the first priority. This may involve:
- Ensuring a clear airway and providing mechanical ventilation if necessary
- Administering intravenous fluids to maintain hydration and electrolyte balance
- Controlling seizures or managing increased intracranial pressure
Targeted Therapies
Once stabilized, targeted treatments aim to reverse or mitigate the effects of the underlying cause:
- Trauma-related comas: Surgery might be required to remove hematomas or relieve pressure on the brain.
- Metabolic disorders: Correcting blood sugar levels, dialysis for kidney failure, or administering antidotes for poisoning.
- Infections: Antibiotics or antiviral medications to combat the source of infection.
Recovery Process
Recovery from a coma is highly variable and depends on several factors, including the cause, duration, and individual patient characteristics. Some individuals regain full consciousness within days, while others may remain in a prolonged state of unconsciousness or transition into a vegetative state.
Phases of Recovery
The recovery process typically follows distinct phases:
- Emergence from coma: Gradual return of basic reflexes and responsiveness to stimuli.
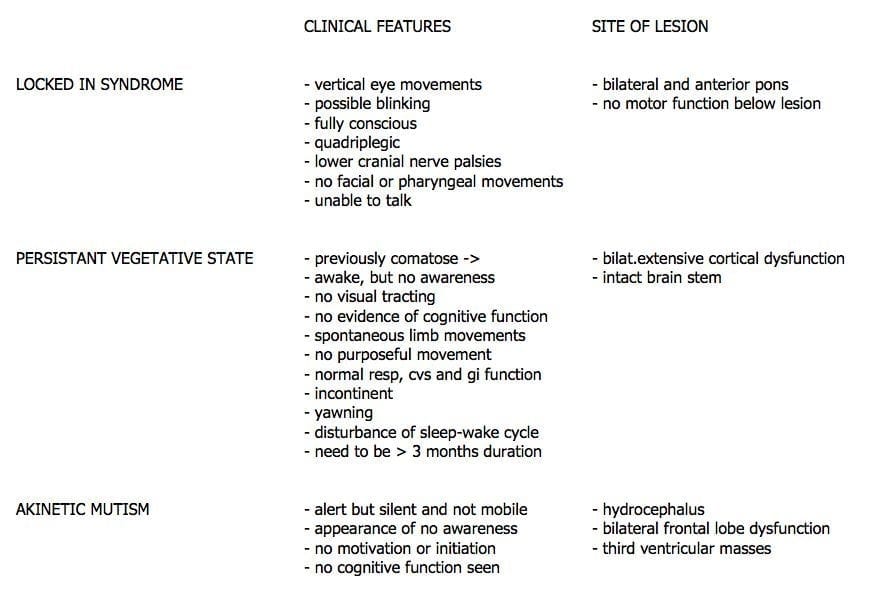
- Vegetative state: Eyes may open, and sleep-wake cycles resume, but awareness remains absent.
- Minimally conscious state: Limited but definite evidence of self-awareness or interaction with the environment.
- Full recovery: Regaining significant cognitive and physical abilities, though residual deficits may persist.
Factors Influencing Recovery
Several elements influence the likelihood and extent of recovery:
- Age and overall health prior to the coma
- Severity and duration of the coma
- Specific area of the brain affected
- Quality and timeliness of medical intervention
Rehabilitation and Support
For those who emerge from a coma, rehabilitation plays a critical role in regaining lost skills and improving quality of life. Physical therapy, occupational therapy, speech therapy, and psychological support are integral components of the recovery journey.
- Physical Therapy: Helps restore mobility, strength, and coordination.
- Occupational Therapy: Focuses on relearning daily activities and adapting to new challenges.
- Speech Therapy: Assists with communication difficulties and swallowing issues.
- Psychological Support: Addresses emotional and mental health needs during recovery.
Long-Term Outcomes
The long-term outcomes of a coma vary widely. While some individuals achieve near-complete recovery, others face permanent disabilities or remain dependent on caregivers. Early and consistent rehabilitation efforts significantly improve the chances of positive outcomes.
Potential Complications
Even after emerging from a coma, patients may encounter complications such as:
- Seizures
- Cognitive impairments
- Emotional and behavioral changes
- Physical disabilities
Family and Caregiver Role
Families and caregivers play a vital role in the recovery process. Their involvement includes providing emotional support, participating in therapy sessions, and making informed decisions about ongoing care.