Colorectal polyps, often abbreviated as CRPs, are growths that develop on the lining of the colon or rectum. These growths can vary in size, shape, and potential to become cancerous. Understanding colorectal polyps is crucial for early detection and prevention of colorectal cancer. This article delves into the types of colorectal polyps, their causes, how they are diagnosed, and the methods used for their removal.
What Are Colorectal Polyps?
Colorectal polyps are abnormal tissue growths that protrude from the inner lining of the large intestine, which includes the colon and rectum. While some polyps remain benign, others have the potential to develop into cancer over time. Early identification and removal of these growths can significantly reduce the risk of developing colorectal cancer.
Why Are Colorectal Polyps Important?
- They are a precursor to colorectal cancer in many cases.
- Early detection and removal can prevent cancer development.
- Understanding their types and causes helps in managing risks effectively.
Types of Colorectal Polyps
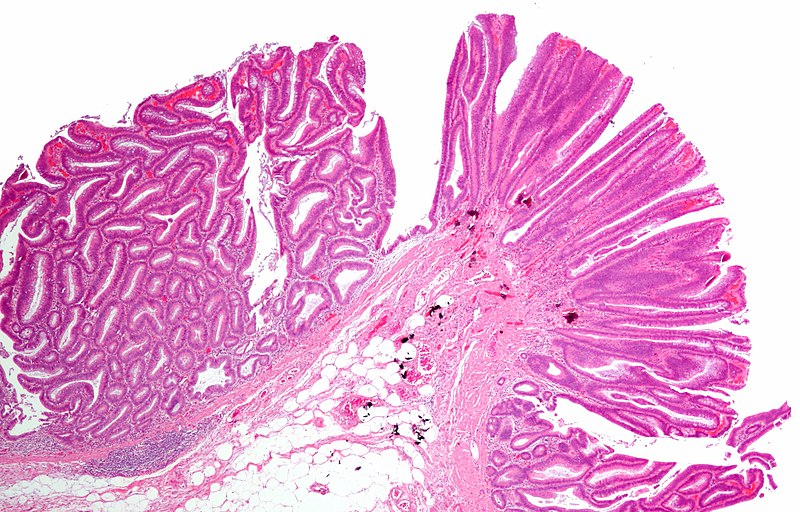
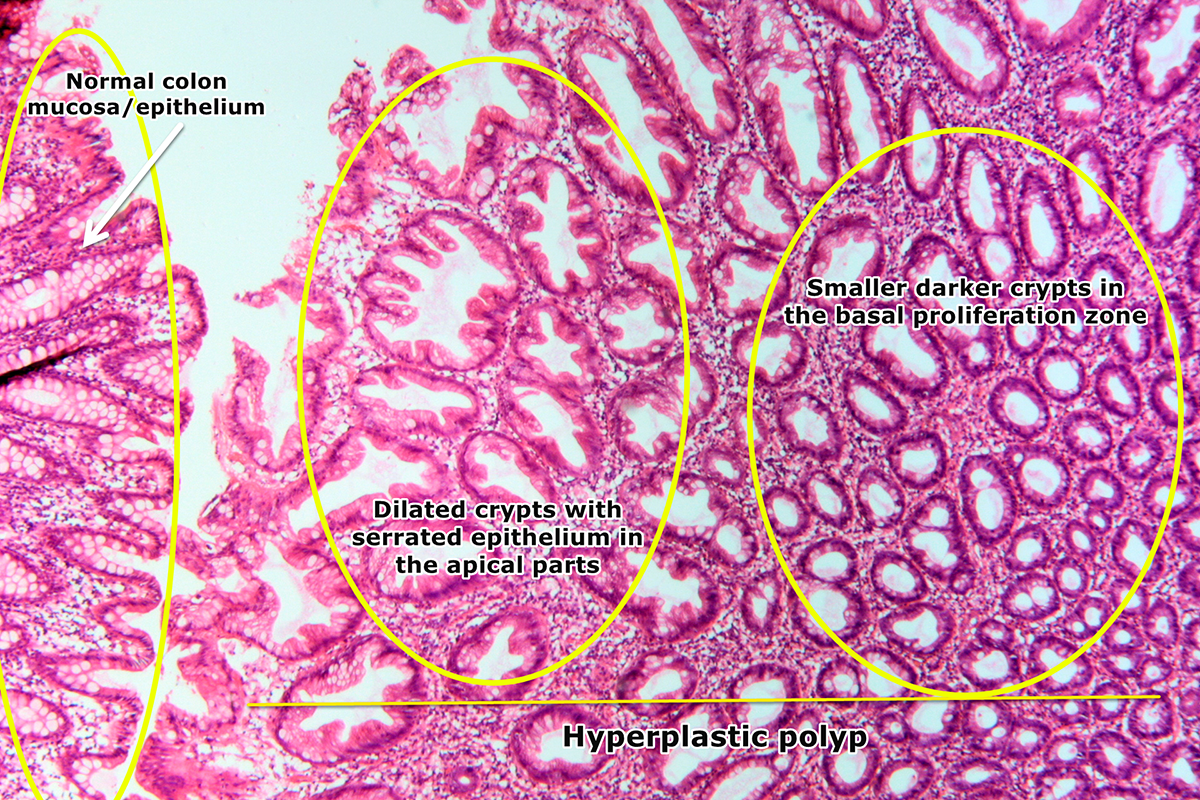
There are several types of colorectal polyps, each with distinct characteristics and levels of risk for becoming cancerous. The classification of polyps is based on their appearance under a microscope and their behavior.
Adenomatous Polyps
Adenomatous polyps are the most common type and are considered precancerous. These growths have the potential to develop into cancer if left untreated. They are further divided into subtypes:
- Tubular adenomas: These are the most common subtype and have a lower risk of becoming cancerous.
- Villous adenomas: These are less common but carry a higher risk of turning into cancer.
- Tubulovillous adenomas: These are a mix of tubular and villous adenomas and have an intermediate risk.
Hyperplastic Polyps
Hyperplastic polyps are usually small and found in the lower part of the colon or rectum. In most cases, they are benign and do not pose a significant cancer risk. However, when they occur in large numbers or in certain locations, they may require closer monitoring.
Inflammatory Polyps
Inflammatory polyps are often associated with inflammatory bowel diseases such as ulcerative colitis or Crohn’s disease. These polyps are generally not precancerous, but their presence indicates ongoing inflammation that needs to be managed.
Serrated Polyps
Serrated polyps have a saw-toothed appearance under the microscope. Some types of serrated polyps, especially those located in the upper colon, can become cancerous if not addressed. They are classified into sessile serrated polyps and traditional serrated adenomas, both of which require careful evaluation.
Causes of Colorectal Polyps
The exact cause of colorectal polyps is not fully understood, but several factors contribute to their development. These include genetic predisposition, lifestyle choices, and underlying health conditions.
Genetic Factors
Some individuals inherit gene mutations that increase their risk of developing colorectal polyps. Conditions such as familial adenomatous polyposis and Lynch syndrome are examples of inherited disorders that lead to the formation of numerous polyps and a high risk of colorectal cancer.
Age
The risk of developing colorectal polyps increases with age. Most cases are diagnosed in individuals over the age of fifty, although younger people can also develop them, especially if they have a family history or other risk factors.
Lifestyle Factors
Certain lifestyle habits can contribute to the development of colorectal polyps. These include:
- A diet high in red meat and processed foods
- Low intake of fiber-rich foods such as fruits, vegetables, and whole grains
- Sedentary lifestyle and lack of physical activity
- Obesity and excess body weight
- Smoking and excessive alcohol consumption
Underlying Health Conditions
Individuals with certain health conditions are at a higher risk of developing colorectal polyps. These conditions include:
- Inflammatory bowel disease, such as ulcerative colitis or Crohn’s disease
- Type 2 diabetes
- History of radiation therapy to the abdomen or pelvis
Diagnosis of Colorectal Polyps
Early diagnosis of colorectal polyps is essential for preventing their progression to cancer. Several screening methods are available to detect these growths before they cause symptoms.
Colonoscopy
A colonoscopy is the gold standard for diagnosing colorectal polyps. During this procedure, a flexible tube with a camera is inserted into the colon to examine its lining. If polyps are found, they can often be removed during the same procedure.
Fecal Occult Blood Test
This test detects hidden blood in the stool, which may indicate the presence of polyps or cancer. While it is not as accurate as a colonoscopy, it is a non-invasive screening option that can prompt further investigation.
Sigmoidoscopy
A sigmoidoscopy is similar to a colonoscopy but only examines the lower part of the colon. It is less comprehensive but can still identify polyps in the rectum and sigmoid colon.
Computed Tomography Colonography
Also known as a virtual colonoscopy, this imaging test uses CT scans to create detailed images of the colon. It is less invasive than a traditional colonoscopy but may require follow-up if abnormalities are detected.
Removal of Colorectal Polyps
Once colorectal polyps are identified, they are typically removed to prevent the development of cancer. The method of removal depends on the size, location, and type of polyp.
Polypectomy
A polypectomy is the most common method of removing polyps during a colonoscopy. Small polyps can be snipped off using a wire loop, while larger polyps may require more advanced techniques.
Endoscopic Mucosal Resection
For larger polyps that cannot be removed with a simple polypectomy, endoscopic mucosal resection may be performed. This procedure involves lifting the polyp away from the colon wall and removing it in sections.
Laparoscopic Surgery
In rare cases where polyps are too large or located in difficult-to-reach areas, laparoscopic surgery may be necessary. This minimally invasive procedure involves making small incisions in the abdomen to remove the polyps.
Follow-Up Care
After polyp removal, regular follow-up screenings are recommended to monitor for new growths. The frequency of these screenings depends on the number, size, and type of polyps removed, as well as the individual’s overall risk factors.
Preventing Colorectal Polyps
While not all colorectal polyps can be prevented, certain measures can reduce the risk of their development. These include adopting a healthy lifestyle, undergoing regular screenings, and managing underlying health conditions.
Dietary Changes
Eating a diet rich in fruits, vegetables, and whole grains while limiting red meat and processed foods can help lower the risk of polyps. Incorporating foods high in fiber and antioxidants is particularly beneficial.
Regular Exercise
Engaging in regular physical activity helps maintain a healthy weight and reduces the risk of colorectal polyps. Aim for at least thirty minutes of moderate exercise most days of the week.
Screening and Early Detection
Regular screenings are critical for detecting polyps early, especially for individuals over the age of fifty or those with a family history of colorectal cancer. Discussing screening options with a healthcare provider can help determine the best approach.