Ulcerative colitis, often abbreviated as UC, is a chronic inflammatory bowel disease that affects the digestive tract. This condition primarily targets the large intestine, also known as the colon, and the rectum. People diagnosed with this disease experience inflammation and ulcers in the lining of their colon, leading to a variety of uncomfortable and sometimes debilitating symptoms. Understanding ulcerative colitis requires a closer look at its symptoms, causes, and available treatments, all of which are essential for managing the condition effectively.
Understanding Ulcerative Colitis
Ulcerative colitis is classified as an autoimmune disorder, meaning the body’s immune system mistakenly attacks healthy cells in the digestive tract. Unlike other forms of inflammatory bowel disease, such as Crohn’s disease, ulcerative colitis only affects the innermost lining of the colon and rectum. The inflammation typically begins in the rectum and may spread continuously through the colon, depending on the severity of the condition.
This disease can occur at any age but is most commonly diagnosed in individuals between the ages of 15 and 30. It is also more prevalent in people of European descent and those with a family history of the condition. While there is no cure for ulcerative colitis, advancements in medical science have made it possible to manage symptoms and improve the quality of life for those affected.
Symptoms of Ulcerative Colitis
The symptoms of ulcerative colitis can vary widely from person to person, depending on the severity and extent of the inflammation. Some individuals may experience mild symptoms, while others may face severe complications. Below are the most common symptoms associated with this condition:
- Frequent Diarrhea: One of the hallmark symptoms of ulcerative colitis is persistent diarrhea, which may contain blood or pus.
- Abdominal Pain and Cramping: Inflammation in the colon can lead to significant discomfort, including sharp pains and cramps in the abdomen.
- Rectal Bleeding: Blood in the stool is a common symptom and may be accompanied by mucus.
- Urgency to Defecate: Many individuals feel a sudden and uncontrollable urge to use the bathroom, even when the bowels are empty.
- Fatigue: Chronic inflammation can cause extreme tiredness and a lack of energy.
- Weight Loss: Unintended weight loss may occur due to reduced appetite or difficulty absorbing nutrients.
- Fever: Low-grade fevers are not uncommon during flare-ups.
In addition to these primary symptoms, some individuals may experience extraintestinal manifestations, which are symptoms that affect areas outside the digestive tract. These can include joint pain, skin rashes, eye inflammation, and liver disorders.
Causes of Ulcerative Colitis
While the exact cause of ulcerative colitis remains unknown, researchers believe it results from a combination of genetic, environmental, and immune system factors. Here’s a closer look at the potential causes:
Genetic Factors
Family history plays a significant role in the development of ulcerative colitis. Studies have shown that individuals with a close relative who has the condition are at a higher risk of developing it themselves. Certain genes have been identified as potentially contributing to the disease, although having these genes does not guarantee that someone will develop ulcerative colitis.
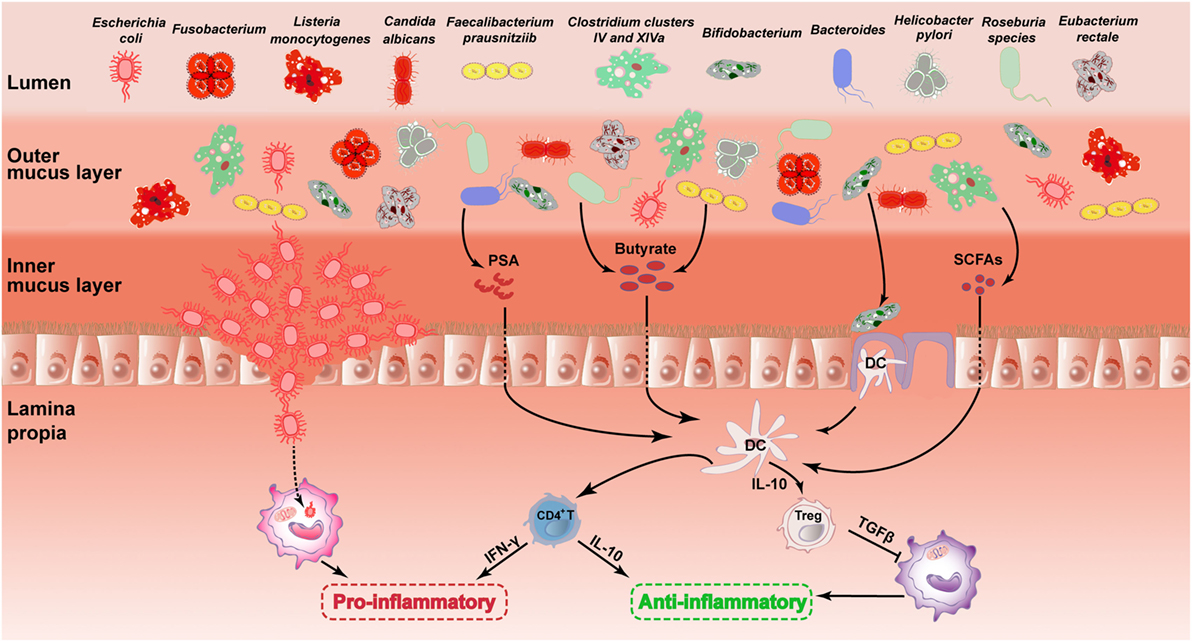
Immune System Dysfunction
Ulcerative colitis is considered an autoimmune disease because the immune system mistakenly attacks the healthy cells lining the colon. Normally, the immune system fights off harmful bacteria and viruses. However, in individuals with ulcerative colitis, the immune response becomes overactive and targets the digestive tract instead. This leads to chronic inflammation and the formation of ulcers.
Environmental Triggers
Several environmental factors may contribute to the onset or worsening of ulcerative colitis. These include:
- Diet: While no specific food has been proven to cause ulcerative colitis, certain foods may trigger symptoms in some individuals.
- Stress: Emotional stress does not cause ulcerative colitis but can exacerbate symptoms during flare-ups.
- Smoking: Interestingly, smoking appears to have a protective effect against ulcerative colitis, although the reasons for this are not fully understood.
- Infections: Some studies suggest that previous gastrointestinal infections may increase the risk of developing the disease.
Treatment Options for Ulcerative Colitis
Although there is no cure for ulcerative colitis, various treatment options are available to help manage symptoms and achieve remission. The goal of treatment is to reduce inflammation, alleviate symptoms, and prevent complications. Treatment plans are highly individualized and depend on the severity of the condition, the location of inflammation, and the patient’s overall health.
Medications
Several types of medications are commonly used to treat ulcerative colitis:
- Aminosalicylates: These anti-inflammatory drugs are often prescribed for mild to moderate cases. They work by reducing inflammation in the colon.
- Corticosteroids: Steroids are used for short-term relief during severe flare-ups. However, they are not suitable for long-term use due to potential side effects.
- Immunomodulators: These medications suppress the immune system to reduce inflammation and are often used for long-term management.
- Biologics: Biologic therapies target specific components of the immune system and are effective for moderate to severe cases.
Dietary and Lifestyle Changes
Making adjustments to diet and lifestyle can significantly improve symptoms and overall well-being:
- Eating a Balanced Diet: Consuming nutrient-rich foods and avoiding trigger foods can help manage symptoms. Common triggers include dairy products, high-fiber foods, and spicy dishes.
- Staying Hydrated: Frequent diarrhea can lead to dehydration, so it’s important to drink plenty of fluids.
- Managing Stress: Techniques such as yoga, meditation, and deep breathing exercises can help reduce stress levels.
- Regular Exercise: Physical activity can improve mood, boost energy levels, and support overall health.
Surgical Interventions
In cases where medication and lifestyle changes are not sufficient, surgery may be necessary. The most common surgical procedure for ulcerative colitis is a proctocolectomy, which involves removing the colon and rectum. After this surgery, patients may require an ileostomy or the creation of an internal pouch to allow for waste elimination.
Living with Ulcerative Colitis
Managing ulcerative colitis requires a proactive approach and ongoing communication with healthcare providers. Regular check-ups, adherence to treatment plans, and monitoring for complications are crucial for maintaining health. Additionally, joining support groups or connecting with others who have the condition can provide emotional support and practical advice.
It’s important to remember that ulcerative colitis affects each person differently. What works for one individual may not work for another, so finding the right combination of treatments and lifestyle adjustments is key. By staying informed and working closely with medical professionals, individuals with ulcerative colitis can lead fulfilling lives despite the challenges posed by the disease.





