Coarctation of the aorta, often abbreviated as CoA, is a congenital heart defect that involves the narrowing of the aorta, the main artery responsible for carrying oxygen-rich blood from the heart to the rest of the body. This condition can significantly impact blood flow and lead to various health complications if not addressed promptly. In this article, we will explore the details of coarctation of the aorta, including its causes, symptoms, diagnostic methods, and available treatments.
Understanding Coarctation of the Aorta
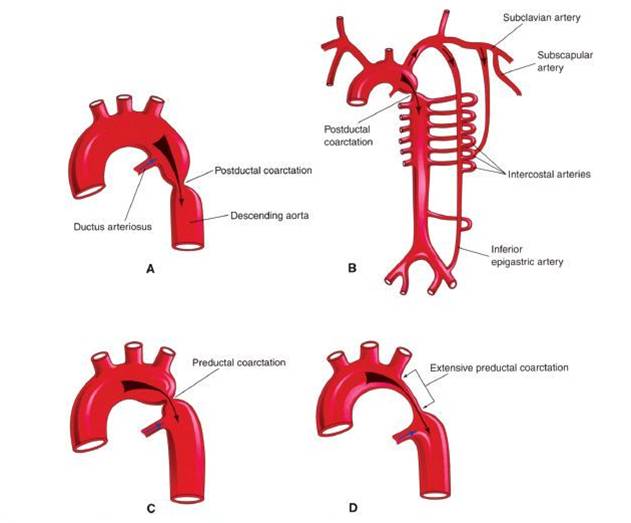
Coarctation of the aorta occurs when a section of the aorta is constricted or narrowed, restricting the normal flow of blood. This narrowing typically happens near the ductus arteriosus, a blood vessel present in the fetus that usually closes shortly after birth. The severity of the condition can vary, with some individuals experiencing mild narrowing while others face more severe obstructions.
Causes and Risk Factors
The exact cause of coarctation of the aorta is not fully understood, but it is believed to develop during fetal growth. Several factors may increase the risk of developing this condition:
- Genetic Factors: Some cases are linked to genetic disorders such as Turner syndrome, a chromosomal condition affecting females.
- Family History: Individuals with a family history of congenital heart defects may have a higher risk of developing coarctation of the aorta.
- Other Heart Defects: Coarctation often occurs alongside other congenital heart problems, such as a bicuspid aortic valve.
Symptoms of Coarctation of the Aorta
The symptoms of coarctation of the aorta can vary depending on the severity of the narrowing and the age at which the condition is diagnosed. In some cases, especially when the narrowing is mild, symptoms may not appear until later in life. However, when symptoms do occur, they may include:
- High Blood Pressure: Individuals with coarctation often experience elevated blood pressure in the arms due to restricted blood flow.
- Weak or Absent Pulses: Reduced blood flow can lead to weak or absent pulses in the legs.
- Cold Extremities: Poor circulation caused by the narrowing can result in cold feet or legs.
- Fatigue: Difficulty in pumping blood efficiently can lead to fatigue and reduced stamina.
- Breathing Difficulties: Infants with severe coarctation may exhibit rapid breathing or difficulty breathing.
- Poor Growth: In children, the condition can lead to poor weight gain and delayed growth.
Symptoms in Infants
In newborns and infants, coarctation of the aorta can present more severe symptoms, especially if the narrowing is significant. These symptoms may include:
- Irritability: Babies may become fussy or irritable due to discomfort.
- Poor Feeding: Difficulty feeding is common, often leading to inadequate nutrition.
- Sweating During Feeding: Excessive sweating, particularly during feeding, can be a sign of heart strain.
- Heart Failure: Severe cases may result in heart failure, characterized by rapid breathing, pale skin, and lethargy.
Diagnosing Coarctation of the Aorta
Early diagnosis of coarctation of the aorta is crucial for effective treatment and management. Healthcare providers use a combination of physical examinations, imaging tests, and other diagnostic tools to identify the condition.
Physical Examination
During a physical examination, a doctor may detect signs of coarctation, such as:
- A noticeable difference in blood pressure between the arms and legs.
- A heart murmur, which is an abnormal sound heard through a stethoscope.
- Weakened or absent pulses in the lower extremities.
Imaging Tests
To confirm the diagnosis, healthcare providers may order one or more imaging tests:
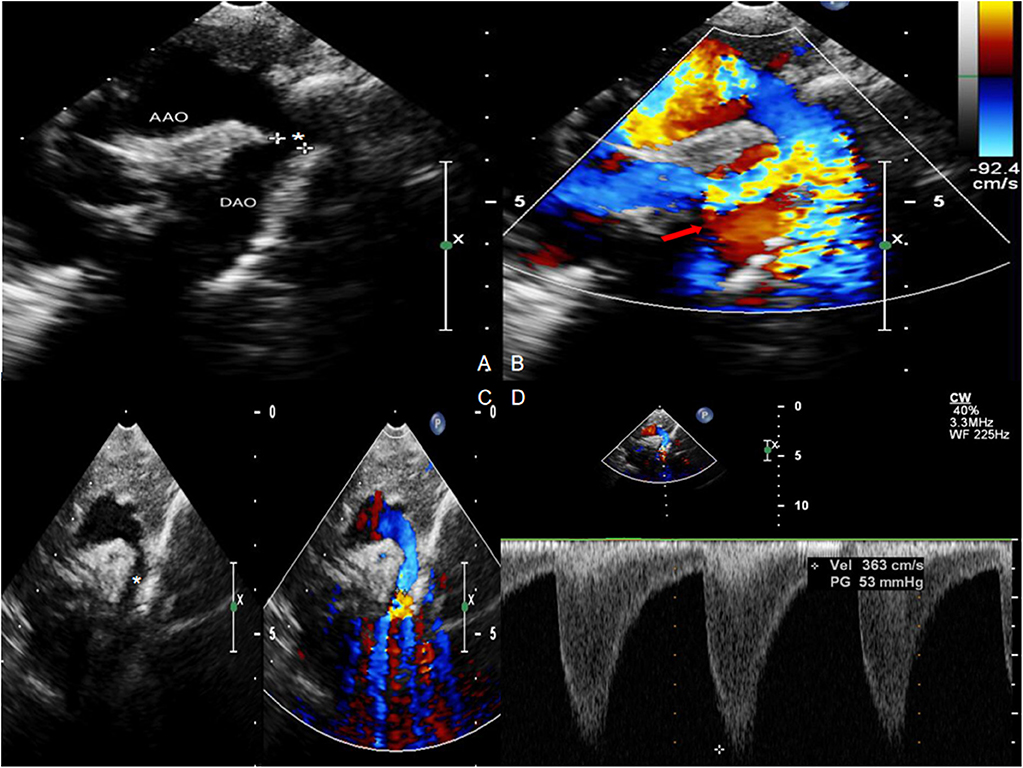
- Echocardiogram: This ultrasound of the heart provides detailed images and helps assess the severity of the narrowing.
- Magnetic Resonance Imaging (MRI): MRI scans can provide a clear picture of the aorta and surrounding structures.
- Computed Tomography (CT) Scan: CT scans offer detailed cross-sectional images of the aorta.
- Chest X-Ray: While not definitive, chest X-rays can reveal an enlarged heart or other abnormalities.
Additional Tests
In some cases, additional tests may be necessary to evaluate the extent of the condition:
- Electrocardiogram (ECG): This test measures the electrical activity of the heart and can detect irregularities.
- Cardiac Catheterization: A minimally invasive procedure where a thin tube is inserted into a blood vessel to measure pressures and assess blood flow.
Treatment Options for Coarctation of the Aorta
Treatment for coarctation of the aorta aims to restore normal blood flow and prevent complications. The approach depends on the severity of the condition, the patient’s age, and overall health. Treatment options include medications, surgical interventions, and minimally invasive procedures.
Medications
In mild cases or as a temporary measure before surgery, medications may be prescribed to manage symptoms and improve heart function:
- Blood Pressure Medications: Drugs such as beta-blockers or ACE inhibitors can help control high blood pressure.
- Diuretics: These medications reduce fluid buildup in the body, easing the workload on the heart.
Surgical Repair
Surgical intervention is often required to correct coarctation of the aorta. The type of surgery depends on the location and severity of the narrowing:
- Resection with End-to-End Anastomosis: The narrowed section of the aorta is removed, and the healthy ends are sewn together.
- Subclavian Flap Aortoplasty: A portion of the subclavian artery is used to widen the narrowed area.
- Patch Aortoplasty: A synthetic patch is used to enlarge the constricted section of the aorta.
Minimally Invasive Procedures
For certain patients, minimally invasive techniques may be an option:
- Balloon Angioplasty: A catheter with a balloon at its tip is used to widen the narrowed section of the aorta.
- Stent Placement: A small mesh tube is inserted to keep the aorta open and maintain proper blood flow.
Lifestyle and Long-Term Management
After treatment, individuals with coarctation of the aorta require ongoing care to monitor their condition and prevent complications. Key aspects of long-term management include:
- Regular Follow-Up Appointments: Routine check-ups with a cardiologist are essential to monitor heart health.
- Blood Pressure Monitoring: Controlling blood pressure is critical to reducing the risk of complications.
- Healthy Lifestyle Choices: Maintaining a balanced diet, exercising regularly, and avoiding smoking contribute to overall cardiovascular health.
Complications Associated with Coarctation of the Aorta
If left untreated, coarctation of the aorta can lead to serious complications, including:
- Heart Failure: The heart may struggle to pump blood effectively, leading to heart failure.
- Hypertension: Chronic high blood pressure can damage organs such as the kidneys and brain.
- Aneurysm Formation: Weakened areas of the aorta may bulge, increasing the risk of rupture.
- Infective Endocarditis: The risk of infection in the heart lining or valves is elevated in individuals with coarctation.
Preventing Complications
Timely diagnosis and treatment play a vital role in preventing complications. Additionally, adhering to medical advice, taking prescribed medications, and attending regular follow-up appointments can significantly reduce risks.