Clostridium difficile, often abbreviated as C. diff, is a bacterium that can cause severe health issues, particularly in the gastrointestinal tract. This article delves into the causes, symptoms, and care associated with this infection, providing an in-depth understanding for those seeking information about this condition.
Understanding Clostridium difficile
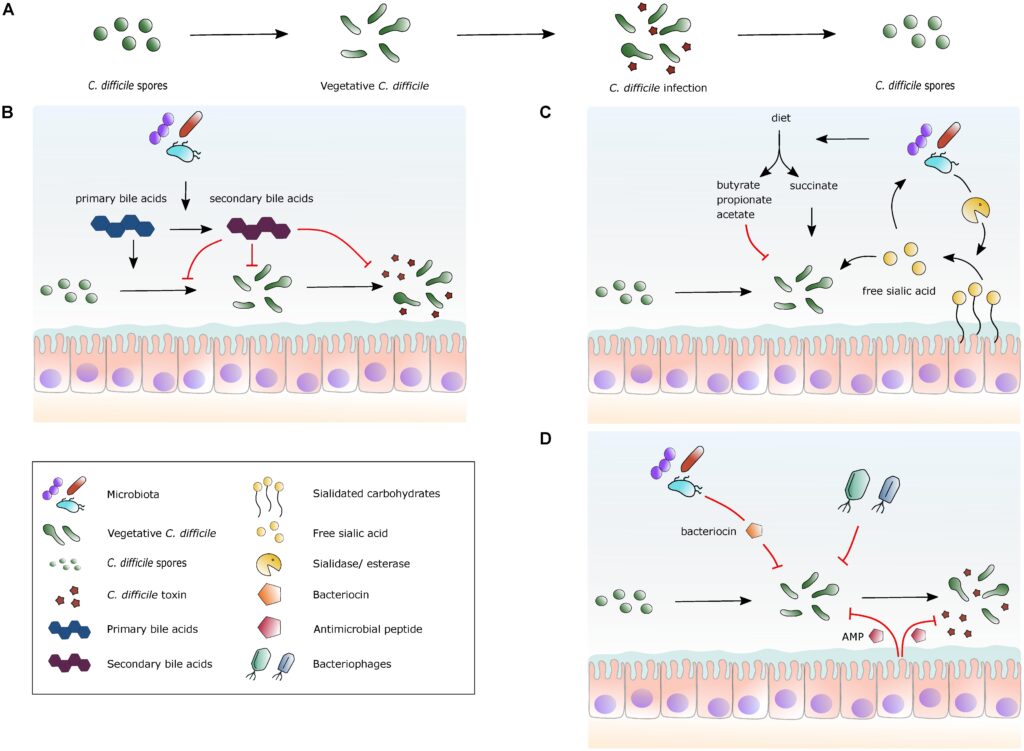
Clostridium difficile is a type of bacteria that resides in the human gut. While it is commonly found in the environment and even in the intestines of healthy individuals, it becomes problematic when it overgrows and releases toxins. These toxins are responsible for causing inflammation and damage to the lining of the colon, leading to a range of symptoms and complications.
How Does Clostridium difficile Spread?
The bacterium spreads primarily through spores, which are highly resistant and can survive on surfaces for extended periods. The following are common ways through which the infection spreads:
- Contact with Contaminated Surfaces: Spores can linger on objects such as doorknobs, bedrails, and medical equipment.
- Poor Hand Hygiene: Failure to wash hands properly after using the restroom or coming into contact with contaminated items can lead to transmission.
- Healthcare Settings: Hospitals and long-term care facilities are common environments where the bacteria spread due to frequent contact between patients and healthcare workers.
Causes of Clostridium difficile Infection
Clostridium difficile infections typically occur when there is an imbalance in the natural bacteria within the gut. Several factors contribute to this imbalance:
Antibiotic Use
One of the primary causes of this infection is the use of antibiotics. While antibiotics are essential for treating bacterial infections, they can also disrupt the balance of beneficial bacteria in the gut. When these beneficial bacteria are reduced, Clostridium difficile has the opportunity to multiply unchecked, releasing harmful toxins.
Weakened Immune System
Individuals with weakened immune systems are more susceptible to infections caused by this bacterium. Conditions such as cancer, HIV/AIDS, and autoimmune disorders can compromise the body’s ability to fight off harmful bacteria, increasing the risk of infection.
Prolonged Hospitalization
Extended stays in healthcare facilities expose individuals to environments where the bacteria are prevalent. Frequent contact with healthcare workers, shared equipment, and close proximity to infected patients all contribute to the spread of the infection.
Symptoms of Clostridium difficile Infection
The symptoms of an infection caused by this bacterium can vary in severity, ranging from mild discomfort to life-threatening complications. Below are the most common symptoms:
Mild Symptoms
- Watery Diarrhea: One of the hallmark signs of infection is frequent, watery stools, often occurring multiple times a day.
- Mild Abdominal Cramping: Individuals may experience discomfort or cramping in the abdominal area.
Severe Symptoms
- Bloody Stools: In more severe cases, stools may contain blood, indicating significant damage to the intestinal lining.
- Severe Abdominal Pain: Intense pain or tenderness in the abdomen can occur as the infection progresses.
- Fever and Dehydration: Elevated body temperature and dehydration are common in severe infections due to fluid loss from diarrhea.
Complications
If left untreated, the infection can lead to serious complications, including:
- Toxic Megacolon: A rare but life-threatening condition where the colon becomes severely inflamed and distended.
- Kidney Failure: Severe dehydration from persistent diarrhea can lead to kidney dysfunction.
- Bowel Perforation: In extreme cases, the infection can cause holes or tears in the walls of the colon.
Diagnosis of Clostridium difficile Infection
Diagnosing this infection involves a combination of clinical evaluation and laboratory testing. Healthcare providers typically assess symptoms and medical history before ordering specific tests to confirm the presence of the bacteria.
Stool Tests
Stool samples are analyzed to detect the presence of toxins produced by the bacteria. These tests are highly sensitive and can provide accurate results within a short period.
Colonoscopy
In some cases, a colonoscopy may be performed to examine the colon directly. This procedure allows healthcare providers to identify areas of inflammation or damage caused by the infection.
Imaging Tests
Imaging techniques such as CT scans or X-rays may be used to assess complications like toxic megacolon or bowel perforation.
Treatment Options for Clostridium difficile Infection
Treatment focuses on eliminating the infection, managing symptoms, and preventing recurrence. The approach depends on the severity of the infection and the patient’s overall health.
Antibiotics
Ironically, antibiotics are used to treat this infection, despite being a primary cause. Specific antibiotics, such as vancomycin or fidaxomicin, are prescribed to target the bacteria without further disrupting the gut flora.
Fecal Microbiota Transplantation
For recurrent or severe cases, fecal microbiota transplantation may be recommended. This procedure involves transferring healthy bacteria from a donor’s stool into the patient’s colon to restore balance to the gut microbiome.
Supportive Care
Managing symptoms and complications is crucial for recovery. Supportive care includes:
- Hydration Therapy: Intravenous fluids may be administered to combat dehydration caused by diarrhea.
- Nutritional Support: A balanced diet rich in probiotics may help restore gut health.
Preventing Clostridium difficile Infection
Prevention plays a critical role in reducing the incidence of this infection. By adopting certain practices, individuals and healthcare facilities can minimize the risk of transmission.
Hand Hygiene
Regular and thorough handwashing with soap and water is one of the most effective ways to prevent the spread of the bacteria. Alcohol-based hand sanitizers are less effective against spores, making traditional handwashing essential.
Environmental Cleaning
Surfaces in healthcare settings should be cleaned regularly with disinfectants specifically designed to kill spores. High-touch areas, such as bedrails and doorknobs, require extra attention.
Antibiotic Stewardship
Healthcare providers are encouraged to prescribe antibiotics judiciously, ensuring they are only used when necessary. This practice helps preserve the balance of beneficial bacteria in the gut.
Vaccination Research
Ongoing research is exploring the development of vaccines to prevent infections caused by this bacterium. While no vaccine is currently available, advancements in this area hold promise for future prevention strategies.
Lifestyle Adjustments for Managing Recurrence
For individuals who experience recurrent infections, lifestyle adjustments can play a vital role in managing the condition and reducing the likelihood of future episodes.
Dietary Changes
Incorporating foods rich in probiotics, such as yogurt and fermented foods, can help restore the balance of gut bacteria. Additionally, avoiding processed foods and excessive sugar may support overall digestive health.
Probiotic Supplements
Some individuals benefit from taking probiotic supplements to replenish beneficial bacteria in the gut. However, it is essential to consult a healthcare provider before starting any supplement regimen.
Stress Management
Chronic stress can weaken the immune system, making individuals more susceptible to infections. Practices such as meditation, yoga, and adequate sleep can help manage stress levels and improve overall well-being.