Liver disease is a growing concern worldwide, and one of its most severe forms is Cirrhosis of the Liver (COL). This condition occurs when healthy liver tissue is replaced by scar tissue, impairing the liver’s ability to function properly. If left untreated, cirrhosis can lead to life-threatening complications. Understanding the causes, recognizing the symptoms, and knowing the diagnostic and treatment options are crucial for managing this condition effectively.
What Is Cirrhosis Of The Liver?
The liver is one of the most vital organs in the human body, responsible for numerous functions such as detoxifying harmful substances, producing bile for digestion, storing energy, and regulating blood clotting. When the liver becomes damaged over time, it attempts to repair itself, leading to the formation of scar tissue. As scar tissue accumulates, the liver’s ability to perform its essential functions diminishes, resulting in cirrhosis.
Cirrhosis is not a disease itself but rather the result of long-term damage caused by various factors. It develops gradually, often over years or even decades, and may go unnoticed until significant damage has occurred.
Causes Of Cirrhosis
Several factors can contribute to the development of cirrhosis. Understanding these causes is key to prevention and early intervention.
Chronic Alcohol Consumption
One of the leading causes of cirrhosis is prolonged and excessive alcohol consumption. Alcohol is toxic to liver cells, and chronic use can lead to inflammation and scarring. Over time, this damage accumulates, eventually progressing to cirrhosis. The risk increases with the amount and duration of alcohol intake.
Viral Hepatitis
Hepatitis B and Hepatitis C are viral infections that cause inflammation of the liver. Chronic infection with either of these viruses can lead to liver damage and ultimately cirrhosis. Hepatitis C, in particular, is a major contributor to cirrhosis cases worldwide.
Fatty Liver Disease
Non-alcoholic fatty liver disease occurs when excess fat builds up in the liver, unrelated to alcohol consumption. This condition is often associated with obesity, diabetes, and high cholesterol levels. Over time, fatty liver disease can progress to inflammation and scarring, leading to cirrhosis.
Autoimmune Disorders
In autoimmune hepatitis, the body’s immune system mistakenly attacks liver cells, causing inflammation and scarring. Primary biliary cholangitis and primary sclerosing cholangitis are other autoimmune conditions that affect the bile ducts and can lead to cirrhosis.
Genetic Disorders
Certain inherited diseases can increase the risk of cirrhosis. These include hemochromatosis, which causes the body to absorb too much iron, and Wilson’s disease, which leads to copper accumulation in the liver. Both conditions can damage liver tissue over time.
Other Causes
- Bile Duct Blockage: Conditions like gallstones or tumors can block bile ducts, leading to bile buildup and liver damage.
- Drugs and Toxins: Certain medications and exposure to environmental toxins can harm the liver.
- Heart Failure: Chronic heart failure can cause fluid buildup in the liver, leading to scarring.
Symptoms Of Cirrhosis
In its early stages, cirrhosis may not cause noticeable symptoms. However, as the condition progresses, signs and symptoms become more apparent. These can vary depending on the severity of the disease.
Early Symptoms
- Fatigue and weakness
- Loss of appetite and weight loss
- Nausea and vomiting
- Abdominal pain and swelling
Advanced Symptoms
- Jaundice, or yellowing of the skin and eyes
- Swelling in the legs and ankles due to fluid retention
- Itchy skin
- Spider-like blood vessels on the skin
- Confusion, difficulty concentrating, or memory problems
- Bleeding or bruising easily
Complications
If left untreated, cirrhosis can lead to serious complications, including:
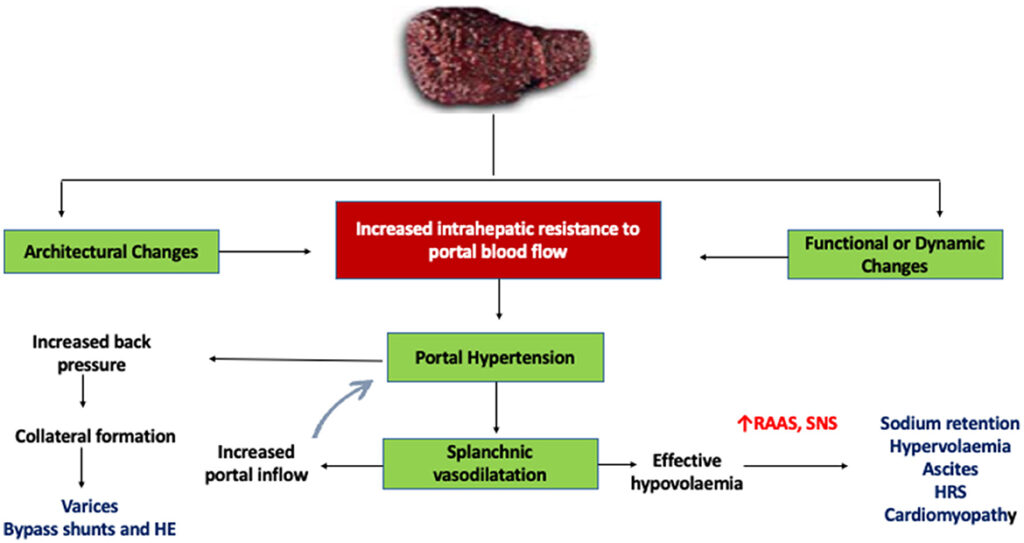
- Portal hypertension, or high blood pressure in the veins that supply the liver
- Ascites, or fluid buildup in the abdomen
- Hepatic encephalopathy, a condition that affects brain function
- Liver cancer
- Kidney failure
Diagnosis Of Cirrhosis
Diagnosing cirrhosis involves a combination of medical history evaluation, physical examination, laboratory tests, imaging studies, and sometimes a liver biopsy.
Medical History and Physical Examination
A healthcare provider will review the patient’s medical history, including alcohol use, medication history, and any underlying health conditions. During the physical exam, they may look for signs such as jaundice, abdominal swelling, or an enlarged liver.
Laboratory Tests
Blood tests can help assess liver function and detect abnormalities. Common tests include:
- Liver function tests to measure enzyme and protein levels
- Complete blood count to check for anemia or low platelet levels
- Tests for viral hepatitis
- Tests to evaluate kidney function
Imaging Studies
Imaging techniques provide detailed pictures of the liver and can help identify scarring or other abnormalities. Common imaging tests include:
- Ultrasound, which uses sound waves to create images
- Computed tomography scans, which provide cross-sectional images
- Magnetic resonance imaging, which offers detailed views of the liver
Liver Biopsy
In some cases, a liver biopsy may be necessary to confirm the diagnosis. During this procedure, a small sample of liver tissue is removed and examined under a microscope to assess the extent of scarring and damage.
Treatment Of Cirrhosis
While cirrhosis cannot be reversed, treatment focuses on slowing its progression, managing symptoms, and preventing complications. The specific approach depends on the underlying cause and the severity of the disease.
Lifestyle Changes
Making lifestyle modifications is essential for managing cirrhosis effectively:
- Abstaining from Alcohol: For individuals with alcohol-related cirrhosis, quitting alcohol is critical to prevent further liver damage.
- Healthy Diet: A balanced diet rich in fruits, vegetables, whole grains, and lean proteins can support liver health. Reducing salt intake can help manage fluid retention.
- Weight Management: Losing excess weight can reduce the risk of fatty liver disease progression.
- Vaccinations: Vaccines for hepatitis A and hepatitis B can protect against additional liver infections.
Medications
Depending on the cause of cirrhosis, medications may be prescribed to manage the condition:
- Antiviral drugs for treating hepatitis B or hepatitis C
- Diuretics to reduce fluid buildup in the abdomen and legs
- Beta-blockers to lower blood pressure in the portal vein
- Lactulose or antibiotics to treat hepatic encephalopathy
Treating Complications
Specific treatments may be required to address complications of cirrhosis:
- Ascites: Paracentesis, a procedure to remove excess fluid from the abdomen, may be necessary.
- Variceal Bleeding: Endoscopic procedures or medications can help control bleeding from enlarged veins in the esophagus or stomach.
- Hepatic Encephalopathy: Medications and dietary changes can improve brain function.
Liver Transplant
In advanced cases where the liver is severely damaged, a liver transplant may be the only option. During this procedure, the diseased liver is replaced with a healthy liver from a donor. While transplantation can be life-saving, it requires lifelong immunosuppressive medications to prevent rejection.
Preventing Cirrhosis
Prevention plays a crucial role in reducing the risk of developing cirrhosis. Key preventive measures include:
- Limiting alcohol consumption or avoiding it altogether
- Getting vaccinated against hepatitis A and hepatitis B
- Maintaining a healthy weight through diet and exercise
- Managing underlying conditions such as diabetes and high cholesterol
- Avoiding unnecessary medications and toxins
Regular check-ups with a healthcare provider can also help detect early signs of liver damage and allow for timely intervention.