Chronic Granulomatous Disease, commonly abbreviated as CGD, is a rare genetic disorder that affects the immune system. This condition leaves individuals vulnerable to recurrent and severe infections caused by certain types of bacteria and fungi. Understanding this disease is crucial for early diagnosis and effective management. In this article, we will explore the causes, symptoms, and care strategies associated with this condition.
What is Chronic Granulomatous Disease?
Chronic Granulomatous Disease is a primary immunodeficiency disorder that impairs the body’s ability to fight off specific infections. People with this condition have immune cells that do not function properly, particularly the white blood cells responsible for destroying harmful microorganisms. As a result, these individuals are prone to developing granulomas, which are clusters of immune cells that form in response to persistent infections or inflammation.
How Does the Immune System Work Normally?
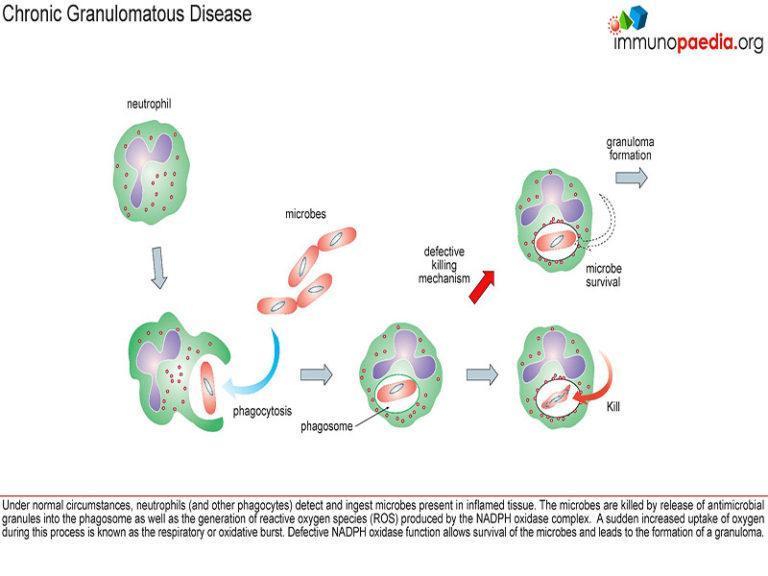
- The immune system protects the body from infections by identifying and neutralizing harmful pathogens like bacteria, viruses, and fungi.
- White blood cells, especially neutrophils, play a critical role in engulfing and destroying these invaders through a process called phagocytosis.
- During phagocytosis, the neutrophils produce reactive oxygen species to kill the engulfed pathogens effectively.
What Happens in Chronic Granulomatous Disease?
- In this disease, the neutrophils fail to produce sufficient reactive oxygen species, leaving them unable to eliminate certain bacteria and fungi.
- This defect leads to recurring infections, often affecting the lungs, skin, lymph nodes, and other organs.
- Additionally, the formation of granulomas can cause blockages in vital organs such as the gastrointestinal tract and urinary system.
Causes of Chronic Granulomatous Disease
This condition is caused by mutations in specific genes that are involved in the functioning of the immune system. These genetic mutations are inherited in an X-linked or autosomal recessive pattern, meaning they can be passed down from one or both parents.
X-Linked Inheritance
- The most common form of this disease is linked to mutations in the CYBB gene, located on the X chromosome.
- Males are more frequently affected because they have only one X chromosome, making them more susceptible if the mutation is present.
- Females can be carriers of the mutation without showing symptoms, but they have a chance of passing it to their children.
Autosomal Recessive Inheritance
- Less commonly, the disease can result from mutations in other genes, such as NCF1, NCF2, or CYBA.
- In autosomal recessive inheritance, both parents must carry a copy of the mutated gene for their child to develop the condition.
- This form of inheritance affects males and females equally.
Symptoms of Chronic Granulomatous Disease
The symptoms of this condition can vary widely depending on the severity of the immune deficiency and the organs affected. However, some common signs and symptoms include:
Recurrent Infections
- Frequent bacterial and fungal infections, particularly those caused by organisms like Staphylococcus aureus, Burkholderia cepacia, and Aspergillus species.
- Pneumonia, lung abscesses, and other respiratory infections are common.
- Skin infections may appear as boils, abscesses, or ulcers.
Granuloma Formation
- Granulomas can develop in various parts of the body, including the skin, liver, spleen, and lymph nodes.
- In the gastrointestinal tract, granulomas may cause symptoms such as abdominal pain, diarrhea, and difficulty swallowing.
- Blockages in the urinary tract can lead to kidney problems or urinary tract infections.
Growth and Development Issues
- Children with this condition may experience delayed growth and development due to chronic illness and inflammation.
- Poor appetite and malnutrition can further contribute to growth delays.
Diagnosis of Chronic Granulomatous Disease
Early diagnosis is essential for managing this condition effectively. Several tests and evaluations can help confirm the presence of this disease.
Laboratory Tests
- A nitroblue tetrazolium test or dihydrorhodamine flow cytometry test can assess the ability of neutrophils to produce reactive oxygen species.
- Blood tests may reveal elevated levels of inflammatory markers, such as C-reactive protein.
- Culture tests can identify specific bacteria or fungi causing infections.
Genetic Testing
- Genetic testing can detect mutations in the genes associated with this condition.
- This type of testing is particularly useful for confirming the diagnosis and identifying carriers within families.
Imaging Studies
- X-rays, CT scans, or MRIs may be used to evaluate the extent of organ involvement and detect granulomas or abscesses.
- These imaging studies are also helpful in monitoring the progression of the disease over time.
Treatment and Care Strategies
While there is no cure for this condition, several treatment options can help manage symptoms and reduce the risk of infections.
Antibiotics and Antifungals
- Prophylactic antibiotics and antifungal medications are often prescribed to prevent infections.
- Trimethoprim-sulfamethoxazole is commonly used to protect against bacterial infections.
- Itraconazole or voriconazole may be prescribed to prevent fungal infections.
Interferon Gamma Therapy
- Interferon gamma injections can enhance the immune response and reduce the frequency of infections.
- This treatment is administered regularly and has been shown to improve outcomes in many patients.
Surgical Interventions
- Surgery may be necessary to remove abscesses, drain infected areas, or address complications caused by granulomas.
- In severe cases, organ transplants may be considered if vital organs are significantly damaged.
Lifestyle and Supportive Care
- A balanced diet rich in nutrients can support overall health and immune function.
- Vaccinations are important to prevent infections from organisms that are not typically associated with this condition.
- Regular follow-ups with healthcare providers are essential for monitoring the disease and adjusting treatment plans as needed.
Living with Chronic Granulomatous Disease
Managing this condition requires a multidisciplinary approach involving healthcare professionals, caregivers, and patients themselves. Education about the disease, adherence to treatment protocols, and a proactive approach to health can significantly improve quality of life.
Emotional and Psychological Support
- Living with a chronic illness can be challenging, and emotional support is crucial for mental well-being.
- Counseling or therapy can help individuals and families cope with the stress and anxiety associated with the condition.
- Support groups provide opportunities to connect with others facing similar challenges and share experiences.
Educating Family Members
- Families should be educated about the genetic nature of the disease and the importance of carrier testing.
- Understanding the risks and implications of inheritance can help in making informed decisions about family planning.
Advances in Research
- Ongoing research into gene therapy and other innovative treatments offers hope for improved outcomes in the future.
- Participating in clinical trials may provide access to cutting-edge therapies and contribute to scientific advancements.