Cholestasis, often abbreviated as CS, refers to a condition where the flow of bile from the liver is interrupted or reduced. This disruption can have significant effects on the body, leading to a range of symptoms and potential complications. In this article, we will delve into the intricacies of cholestasis, exploring its causes, symptoms, diagnosis, and treatment options.
What is Cholestasis?
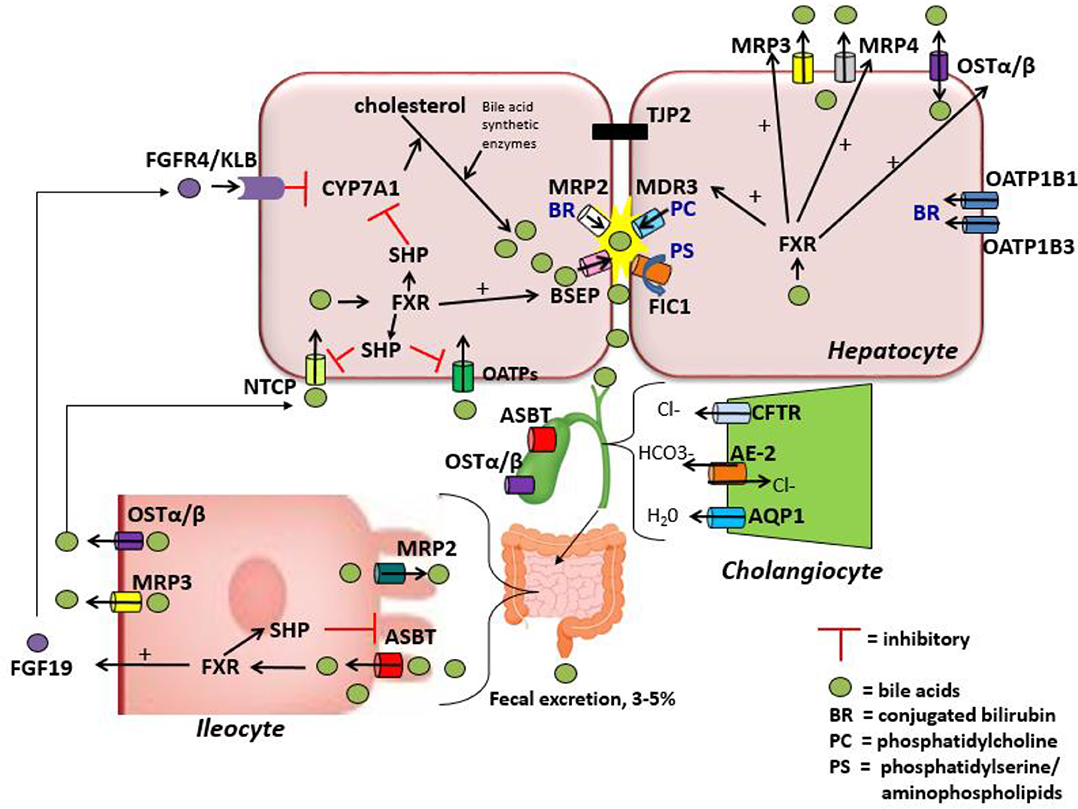
Cholestasis occurs when there is a blockage or reduction in the flow of bile, a digestive fluid produced by the liver. Bile plays a crucial role in digestion, particularly in the breakdown and absorption of fats. When bile flow is impeded, it can lead to a buildup of bile components in the liver, causing damage and affecting overall health.
Types of Cholestasis
- Intrahepatic Cholestasis: This type occurs within the liver and is often caused by issues such as liver disease, infections, or certain medications.
- Extrahepatic Cholestasis: This type occurs outside the liver, typically due to blockages in the bile ducts, such as gallstones or tumors.
Causes of Cholestasis
The causes of cholestasis can be varied and depend on whether the condition is intrahepatic or extrahepatic.
Intrahepatic Causes
- Liver Diseases: Conditions such as hepatitis, cirrhosis, and primary biliary cirrhosis can lead to intrahepatic cholestasis.
- Infections: Viral infections like hepatitis A, B, and C can cause inflammation and disrupt bile flow.
- Medications: Certain drugs, including antibiotics and anabolic steroids, can impair bile production or flow.
Extrahepatic Causes
- Gallstones: These are solid particles that form in the gallbladder and can block the bile ducts.
- Tumors: Cancerous growths in the bile ducts or pancreas can obstruct bile flow.
- Biliary Atresia: A congenital condition where bile ducts are absent or damaged, leading to cholestasis in infants.
Symptoms of Cholestasis
The symptoms of cholestasis can vary depending on the underlying cause and severity of the condition. Common symptoms include:
- Jaundice: Yellowing of the skin and eyes due to a buildup of bilirubin.
- Dark Urine: The presence of excess bilirubin in the urine can cause it to appear darker than usual.
- Pale Stools: Bile is responsible for the brown color of stools; its absence can lead to pale or clay-colored stools.
- Itching: Known as pruritus, this is a common symptom caused by bile salts accumulating under the skin.
- Fatigue: General tiredness and weakness can occur as the body struggles to digest fats properly.
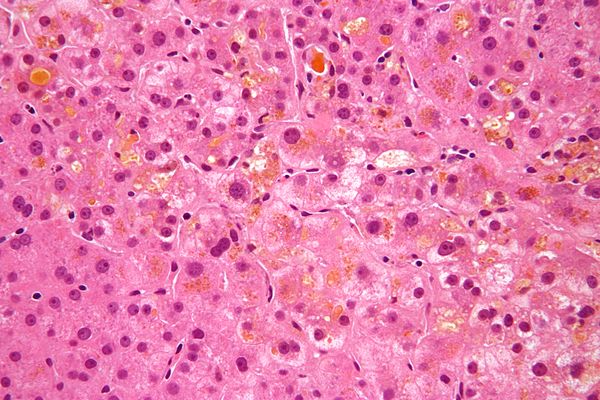
Diagnosis of Cholestasis
Diagnosing cholestasis involves a combination of clinical evaluation, laboratory tests, and imaging studies.
Clinical Evaluation
A healthcare provider will begin by taking a detailed medical history and conducting a physical examination. They will look for signs of jaundice, liver enlargement, and other symptoms associated with cholestasis.
Laboratory Tests
- Liver Function Tests: These tests measure levels of liver enzymes, bilirubin, and other substances to assess liver health.
- Blood Tests: Additional blood tests may be performed to check for infections, autoimmune conditions, or other underlying causes.
Imaging Studies
- Ultrasound: This non-invasive test uses sound waves to create images of the liver and bile ducts, helping identify blockages or abnormalities.
- Magnetic Resonance Imaging: MRI scans provide detailed images of the liver and bile ducts, useful for detecting tumors or strictures.
- Endoscopic Retrograde Cholangiopancreatography: This procedure combines endoscopy and X-rays to visualize the bile ducts and remove any blockages if necessary.
Treatment Options for Cholestasis
Treatment for cholestasis focuses on addressing the underlying cause and managing symptoms. The approach may vary depending on whether the condition is intrahepatic or extrahepatic.
Addressing Underlying Causes
- Medication Adjustment: If cholestasis is caused by medications, adjusting the dosage or switching to alternative treatments may help.
- Infection Treatment: Treating viral or bacterial infections with appropriate medications can resolve cholestasis.
- Surgical Intervention: In cases of gallstones or tumors, surgery may be necessary to remove obstructions and restore bile flow.
Managing Symptoms
- Ursodeoxycholic Acid: This medication helps improve bile flow and reduce itching associated with cholestasis.
- Vitamin Supplementation: Patients with cholestasis may require supplements for fat-soluble vitamins like A, D, E, and K.
- Antihistamines: These can help alleviate itching by blocking histamine receptors in the skin.
Complications of Cholestasis
If left untreated, cholestasis can lead to several complications, including:
- Liver Damage: Prolonged bile accumulation can cause inflammation and scarring of the liver, leading to cirrhosis.
- Osteoporosis: Reduced absorption of vitamin D and calcium can weaken bones and increase the risk of fractures.
- Nutritional Deficiencies: Impaired fat digestion can result in deficiencies of essential fatty acids and fat-soluble vitamins.
Living with Cholestasis
Managing cholestasis requires a comprehensive approach that includes lifestyle modifications, regular monitoring, and adherence to treatment plans.
Dietary Considerations
- Low-Fat Diet: Reducing fat intake can help manage symptoms and improve digestion.
- Hydration: Staying well-hydrated supports liver function and overall health.
- Supplements: Ensuring adequate intake of vitamins and minerals through diet or supplements is crucial.
Regular Monitoring
Patients with cholestasis should undergo regular check-ups to monitor liver function and adjust treatment as needed. This includes periodic blood tests and imaging studies to track the progression of the condition.
Emotional Support
Living with a chronic condition like cholestasis can be challenging. Seeking support from healthcare providers, support groups, and loved ones can help manage the emotional and psychological aspects of the disease.
Emerging Research and Future Directions
Research into cholestasis is ongoing, with scientists exploring new treatments and therapies to improve outcomes for patients. Some promising areas of research include:
- Gene Therapy: Investigating genetic factors involved in cholestasis could lead to targeted treatments.
- Novel Medications: Developing new drugs that enhance bile flow and protect liver cells is a key focus.
- Stem Cell Therapy: Exploring the potential of stem cells to regenerate damaged liver tissue offers hope for future treatments.
Understanding the complexities of cholestasis and staying informed about advancements in treatment can empower patients and healthcare providers to better manage this challenging condition.