Cervical stenosis, often abbreviated as CS, is a medical condition that involves the narrowing of the spinal canal in the neck region. This narrowing can lead to compression of the spinal cord and nerve roots, resulting in various symptoms that affect daily life. In this article, we will explore the causes, symptoms, diagnosis, and treatment options for this condition, providing a comprehensive understanding of cervical stenosis.
What is Cervical Stenosis?
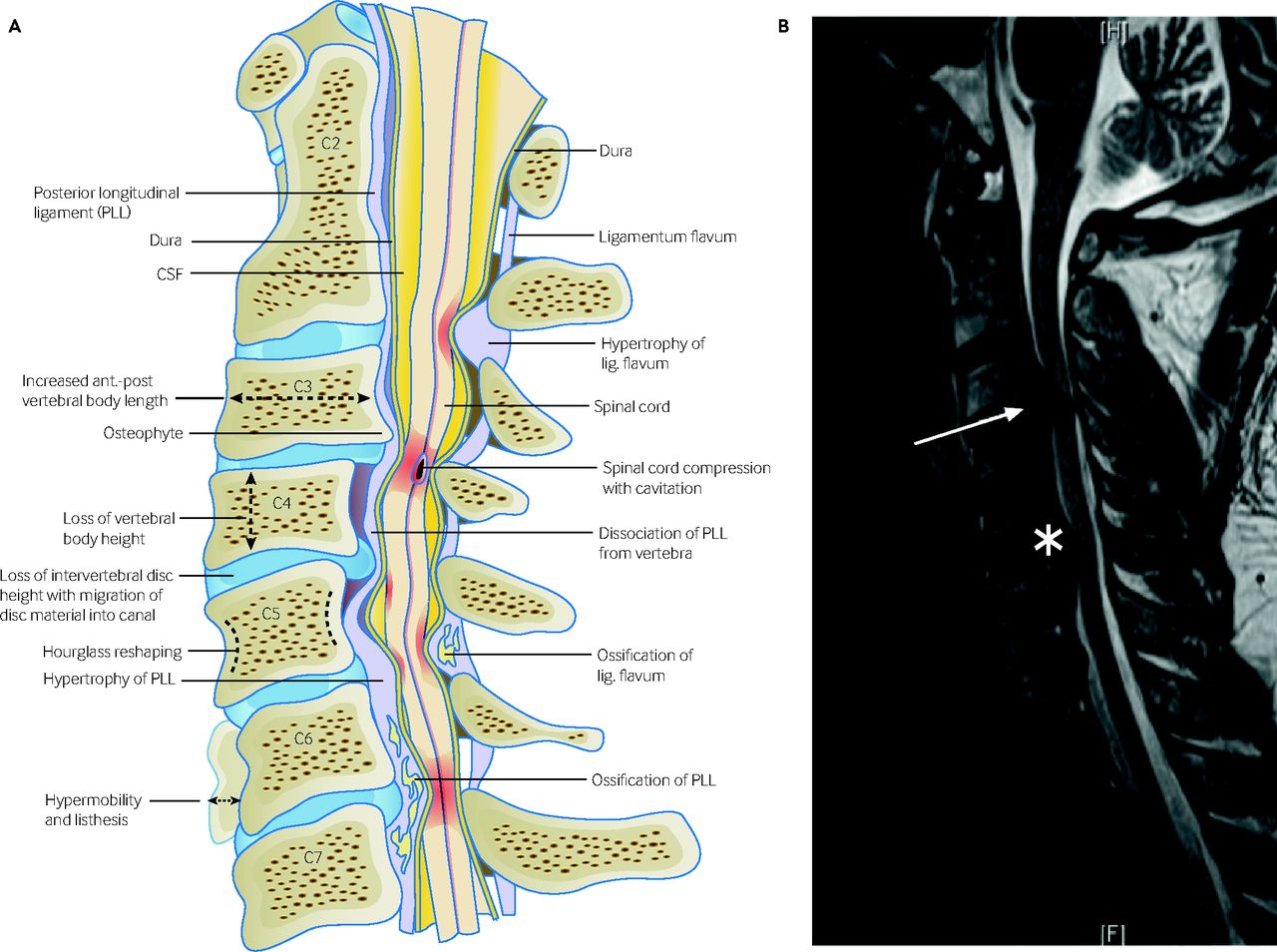
The spinal canal is a hollow space within the spine that houses the spinal cord and nerve roots. In the neck area, known as the cervical spine, this canal can become narrower over time due to various factors. When this happens, it puts pressure on the spinal cord and nerves, leading to a range of symptoms. Cervical stenosis is most commonly seen in older adults, but it can also occur in younger individuals due to congenital factors or injuries.
Causes of Cervical Stenosis
Several factors can contribute to the development of cervical stenosis. These include:
- Age-related changes: As people age, the structures of the spine can degenerate. The discs between the vertebrae may lose water content and shrink, leading to reduced space within the spinal canal. Bone spurs may also form, further narrowing the canal.
- Herniated discs: Discs act as cushions between the vertebrae. When a disc herniates, its inner material can protrude into the spinal canal, causing compression of the spinal cord or nerves.
- Injuries: Trauma to the neck, such as fractures or dislocations, can damage the spinal canal and lead to stenosis.
- Congenital factors: Some individuals are born with a naturally narrow spinal canal, making them more susceptible to developing cervical stenosis later in life.
- Ligament thickening: Over time, ligaments that support the spine can thicken and stiffen, encroaching on the spinal canal.
Symptoms of Cervical Stenosis
The symptoms of cervical stenosis can vary depending on the severity of the narrowing and the specific nerves affected. Common symptoms include:
- Pain: Individuals may experience pain in the neck, shoulders, arms, or hands. This pain can be sharp, dull, or burning and may radiate down the arms.
- Numbness or tingling: Compression of the nerves can cause sensations of numbness or tingling in the arms, hands, or fingers.
- Weakness: Muscle weakness in the arms or hands may occur, affecting grip strength and fine motor skills.
- Bowel or bladder dysfunction: In severe cases, cervical stenosis can lead to problems with bowel or bladder control, which requires immediate medical attention.
- Balance issues: Some individuals may experience difficulty walking or maintaining balance due to spinal cord compression.
Diagnosing Cervical Stenosis
Diagnosing cervical stenosis typically involves a combination of physical examinations, medical history reviews, and imaging tests. Here is an overview of the diagnostic process:
Physical Examination
A healthcare provider will begin by conducting a thorough physical examination. They will assess the patient’s range of motion, reflexes, muscle strength, and sensation in the arms and legs. Any signs of nerve compression, such as weakness or numbness, will be noted.
Medical History
Understanding the patient’s medical history is crucial in diagnosing cervical stenosis. The healthcare provider will inquire about any previous injuries, surgeries, or conditions that may have contributed to the development of the condition. They will also ask about the onset and progression of symptoms.
Imaging Tests
Imaging tests play a key role in confirming the presence of cervical stenosis and determining its severity. Common imaging techniques include:
- X-rays: X-rays can reveal changes in the bones of the spine, such as bone spurs or fractures, but they do not provide detailed images of soft tissues like discs or nerves.
- Magnetic resonance imaging: Magnetic resonance imaging provides detailed images of the spine, including the spinal cord, discs, and nerves. It is considered the gold standard for diagnosing cervical stenosis.
- Computed tomography scans: Computed tomography scans use X-rays to create cross-sectional images of the spine. They are particularly useful for visualizing bone structures and identifying areas of narrowing.
- Myelogram: A myelogram involves injecting a contrast dye into the spinal canal before taking X-rays or computed tomography scans. This test helps highlight areas where the spinal cord or nerves are compressed.
Treatment Options for Cervical Stenosis
The treatment for cervical stenosis depends on the severity of the condition and the symptoms experienced by the patient. Treatment options range from conservative measures to surgical interventions.
Conservative Treatments
For mild cases of cervical stenosis, non-surgical treatments may be sufficient to manage symptoms. These include:
- Physical therapy: Physical therapy focuses on strengthening the muscles around the neck and improving flexibility. Exercises can help alleviate pain and improve posture.
- Medications: Nonsteroidal anti-inflammatory drugs can reduce inflammation and relieve pain. In some cases, muscle relaxants or nerve pain medications may be prescribed.
- Epidural steroid injections: These injections deliver corticosteroids directly into the epidural space around the spinal cord, reducing inflammation and relieving pain.
- Activity modification: Avoiding activities that exacerbate symptoms, such as heavy lifting or repetitive neck movements, can help prevent further irritation.
Surgical Treatments
If conservative treatments fail to provide relief or if the condition is severe, surgery may be necessary. Surgical options for cervical stenosis include:
- Decompression surgery: This procedure involves removing parts of the bone, ligaments, or discs that are compressing the spinal cord or nerves. Common decompression surgeries include laminectomy and foraminotomy.
- Spinal fusion: Spinal fusion involves joining two or more vertebrae together to stabilize the spine. This procedure is often performed in conjunction with decompression surgery to prevent instability.
- Artificial disc replacement: In some cases, a damaged disc may be replaced with an artificial one to restore normal function and reduce pain.
Risks and Recovery from Surgery
While surgery can effectively relieve symptoms of cervical stenosis, it is not without risks. Potential complications include infection, bleeding, nerve damage, and failure to relieve symptoms. Recovery from surgery varies depending on the type of procedure performed and the individual’s overall health. Physical therapy is often recommended post-surgery to aid in recovery and restore function.
Living with Cervical Stenosis
Managing cervical stenosis often requires lifestyle adjustments to minimize symptoms and prevent further progression of the condition. Here are some tips for living with cervical stenosis:
Maintaining Good Posture
Poor posture can exacerbate symptoms of cervical stenosis. Practicing good posture, especially when sitting or using electronic devices, can help reduce strain on the neck and spine.
Regular Exercise
Engaging in regular low-impact exercises, such as swimming, walking, or yoga, can help maintain flexibility and strengthen the muscles supporting the spine.
Ergonomic Adjustments
Making ergonomic adjustments at work or home, such as using a supportive chair or adjusting computer screens to eye level, can reduce stress on the neck and improve comfort.
Stress Management
Stress can contribute to muscle tension and worsen symptoms of cervical stenosis. Incorporating relaxation techniques, such as deep breathing, meditation, or mindfulness, can help manage stress levels.





