Cervical cancer, often abbreviated as CC, is a significant health concern for women worldwide. It is one of the most common types of cancer affecting the female reproductive system. Despite advancements in medical science, cervical cancer remains a leading cause of mortality among women, particularly in low- and middle-income countries. This article delves into the causes, symptoms, and treatments associated with this disease to provide a comprehensive understanding of its impact on health.

What is Cervical Cancer?
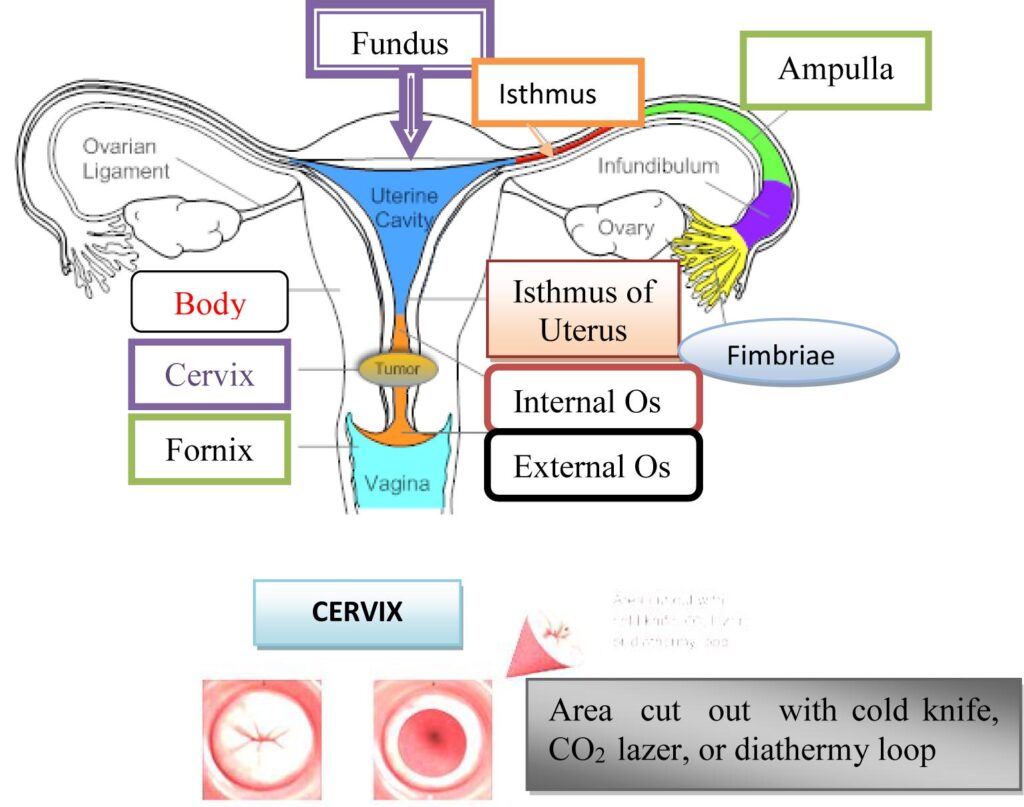
Cervical cancer originates in the cells of the cervix, which is the lower part of the uterus that connects to the vagina. The cervix plays a vital role in the female reproductive system, allowing menstrual blood to flow out of the uterus and enabling sperm to travel into the uterus during conception. When abnormal cells in the cervix grow uncontrollably, they can form tumors that may eventually spread to other parts of the body if left untreated.
Types of Cervical Cancer
- Squamous Cell Carcinoma: This type accounts for approximately eighty to ninety percent of all cases and develops in the thin, flat cells lining the outer part of the cervix.
- Adenocarcinoma: This type arises from the glandular cells that produce mucus in the cervical canal. It is less common but still significant.
- Mixed Carcinoma: In some cases, both squamous cells and glandular cells are involved in the development of cancer.
Causes of Cervical Cancer
The primary cause of cervical cancer is persistent infection with high-risk types of the human papillomavirus. However, several other factors can contribute to the development of this disease.
Role of Human Papillomavirus
The human papillomavirus is a group of more than one hundred related viruses, some of which are considered high-risk due to their association with cancer. High-risk types, such as sixteen and eighteen, are responsible for the majority of cervical cancer cases. These viruses infect the cells of the cervix and can lead to changes in the DNA of these cells, causing them to grow abnormally.
Risk Factors
- Weak Immune System: Individuals with weakened immune systems, such as those with HIV or those who have undergone organ transplants, are at higher risk.
- Smoking: Smoking increases the risk of developing cervical cancer by damaging the DNA of cervical cells and weakening the immune response.
- Multiple Sexual Partners: Engaging in sexual activity with multiple partners increases the likelihood of exposure to the human papillomavirus.
- Early Sexual Activity: Becoming sexually active at a young age can increase the risk of infection with the virus.
- Long-Term Use of Birth Control Pills: Studies suggest that prolonged use of oral contraceptives may slightly elevate the risk of cervical cancer.
- Socioeconomic Factors: Women in low-income communities often lack access to regular screenings and preventive care, increasing their vulnerability.
Symptoms of Cervical Cancer
In its early stages, cervical cancer often does not present noticeable symptoms. This is why regular screenings are crucial for early detection. However, as the disease progresses, certain signs may become apparent.
Common Symptoms
- Abnormal Vaginal Bleeding: This includes bleeding between periods, after sexual intercourse, or after menopause.
- Pelvic Pain: Persistent pain in the pelvic region may indicate an underlying issue.
- Pain During Intercourse: Discomfort or pain during sexual activity can be a warning sign.
- Vaginal Discharge: Unusual discharge that may be watery, bloody, or have a foul odor.
Advanced Symptoms
As cervical cancer spreads to nearby tissues or organs, additional symptoms may arise:
- Swelling in the Legs: This occurs when cancer obstructs the lymphatic system.
- Kidney Problems: Blockage of the urinary tract can lead to kidney failure.
- Bone Pain: If cancer metastasizes to the bones, it can cause severe pain.
Diagnosis of Cervical Cancer
Early diagnosis is critical for improving outcomes. Several methods are used to detect and diagnose cervical cancer.
Pap Smear Test
A Pap smear test involves collecting cells from the surface of the cervix to check for abnormalities. It is recommended that women begin regular Pap smears at the age of twenty-one and continue every three years, depending on their health history.
Human Papillomavirus Testing
This test detects the presence of high-risk types of the virus in cervical cells. It is often performed alongside a Pap smear for women over thirty or for those with abnormal Pap results.
Colposcopy
If abnormalities are detected during a Pap smear, a colposcopy may be performed. This procedure uses a special magnifying instrument to examine the cervix more closely.
Biopsy
A biopsy involves removing a small sample of cervical tissue for laboratory analysis. This is the definitive method for diagnosing cervical cancer.
Treatment Options for Cervical Cancer
The treatment of cervical cancer depends on the stage of the disease, the patient’s overall health, and personal preferences. Below are the primary treatment modalities available.
Surgery
Surgical intervention is often the first line of treatment for early-stage cervical cancer.
- Cone Biopsy: This procedure removes a cone-shaped piece of tissue from the cervix and is often used for very early-stage cancers.
- Hysterectomy: A hysterectomy involves the removal of the uterus and, in some cases, the surrounding tissues. It may be partial or complete, depending on the extent of the cancer.
- Lymph Node Removal: Nearby lymph nodes may also be removed to check for the spread of cancer.
Radiation Therapy
Radiation therapy uses high-energy beams to destroy cancer cells. It can be administered externally or internally and is often combined with chemotherapy for advanced cases.
Chemotherapy
Chemotherapy involves the use of drugs to kill cancer cells. It is typically used for advanced or recurrent cervical cancer and is often paired with radiation therapy to enhance effectiveness.
Targeted Therapy
Targeted therapy focuses on specific vulnerabilities within cancer cells. For example, drugs like bevacizumab target the blood vessels that supply tumors, cutting off their nutrient supply.
Immunotherapy
Immunotherapy harnesses the body’s immune system to fight cancer. This approach is still being researched but shows promise for treating advanced cervical cancer.
Prevention of Cervical Cancer
Preventive measures play a crucial role in reducing the incidence of cervical cancer. These include vaccination, lifestyle changes, and regular screenings.
Vaccination
The human papillomavirus vaccine is highly effective in preventing infection with high-risk types of the virus. It is recommended for both boys and girls aged eleven to twelve, although it can be administered up to age twenty-six.
Healthy Lifestyle Choices
Quitting smoking, practicing safe sex, and maintaining a strong immune system through a balanced diet and regular exercise can significantly reduce the risk of developing cervical cancer.
Regular Screenings
Regular Pap smears and human papillomavirus testing are essential for early detection and prevention. Women should follow the recommended screening guidelines based on their age and health history.
Living with Cervical Cancer
A diagnosis of cervical cancer can be overwhelming, but support is available. Counseling, support groups, and educational resources can help patients and their families navigate the emotional and practical challenges of living with the disease.
Emotional Support
Many women find comfort in connecting with others who are going through similar experiences. Support groups, both in-person and online, provide a platform for sharing stories and coping strategies.
Managing Side Effects
Treatments for cervical cancer can cause side effects such as fatigue, nausea, and hair loss. Working closely with healthcare providers can help manage these symptoms and improve quality of life.
Nutrition and Wellness
A healthy diet and regular physical activity can boost energy levels and support recovery. Patients are encouraged to consult with nutritionists to develop personalized meal plans.