Whipple’s Disease, often abbreviated as WD, is a rare and complex condition that affects multiple systems in the body. Despite its rarity, understanding this disease is crucial for early diagnosis and effective treatment. This article delves into the symptoms, diagnostic methods, and treatment options available for those affected by this challenging illness.
Understanding Whipple’s Disease
Whipple’s Disease is a bacterial infection caused by Tropheryma whipplei. This bacterium primarily targets the digestive system but can also affect other parts of the body, including the heart, lungs, brain, and joints. The disease was first described in 1907 by George Hoyt Whipple, and since then, it has remained a subject of medical interest due to its elusive nature and varied presentation.
The Cause of Whipple’s Disease
The primary cause of this condition is the bacterium Tropheryma whipplei. While many people may carry this bacterium without developing symptoms, certain individuals are more susceptible to its effects. Factors such as genetic predisposition, immune system deficiencies, and environmental influences may contribute to the onset of the disease.
Symptoms of Whipple’s Disease
The symptoms of this condition can vary widely, making it difficult to diagnose. They often mimic other diseases, leading to delays in proper treatment. Below are the most common symptoms associated with the disease:
Gastrointestinal Symptoms
- Chronic diarrhea
- Abdominal pain and cramping
- Weight loss and malnutrition
- Fatty stools, also known as steatorrhea
Systemic Symptoms
- Fever and night sweats
- Fatigue and weakness
- Joint pain and swelling
- Anemia
Neurological Symptoms
- Memory loss and cognitive decline
- Difficulty with coordination and balance
- Vision problems
- Seizures
Cardiovascular Symptoms
- Endocarditis, or inflammation of the heart lining
- Heart murmurs
- Chest pain
Diagnosis of Whipple’s Disease
Diagnosing this condition can be challenging due to its nonspecific symptoms and the rarity of the disease. However, several diagnostic tools and techniques are available to help identify the presence of the bacterium and confirm the diagnosis.
Clinical Evaluation
A thorough clinical evaluation is the first step in diagnosing the condition. Physicians will review the patient’s medical history, conduct a physical examination, and assess the symptoms presented. This initial assessment helps narrow down potential causes and guides further testing.
Laboratory Tests
- Blood Tests: Blood tests may reveal signs of anemia, inflammation, or malnutrition. These findings can support the suspicion of the disease but are not definitive on their own.
- Stool Analysis: Examination of stool samples can detect the presence of fat, which indicates malabsorption issues commonly seen in this condition.
Imaging Studies
- X-rays and CT Scans: Imaging studies may show thickening of the intestinal walls or other abnormalities in the digestive tract.
- MRI: Magnetic resonance imaging can help identify neurological involvement, such as brain lesions or inflammation.
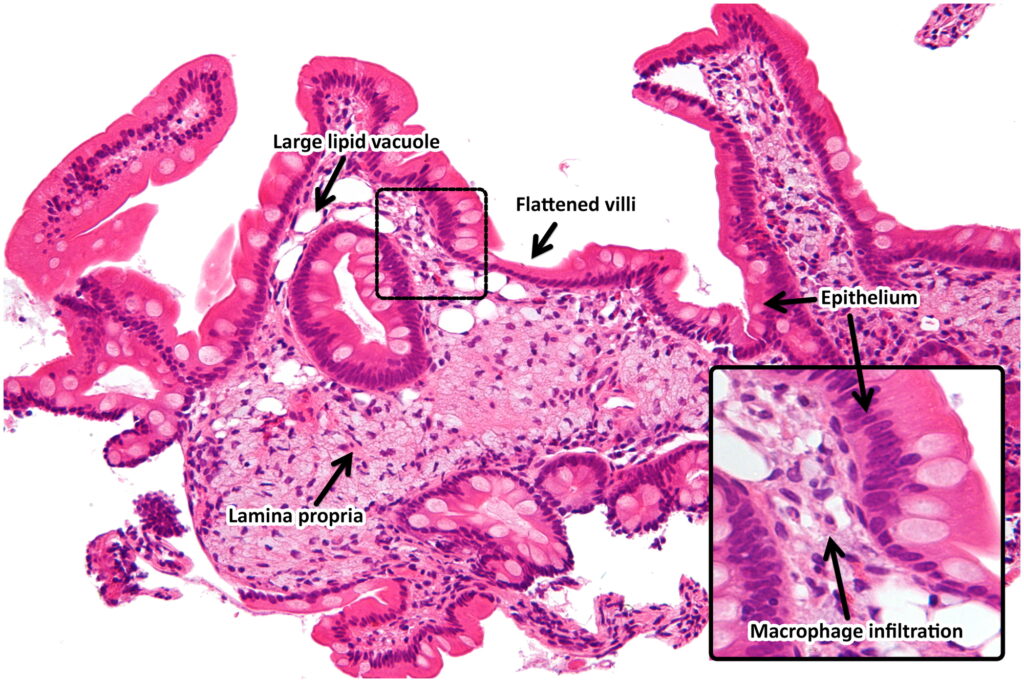
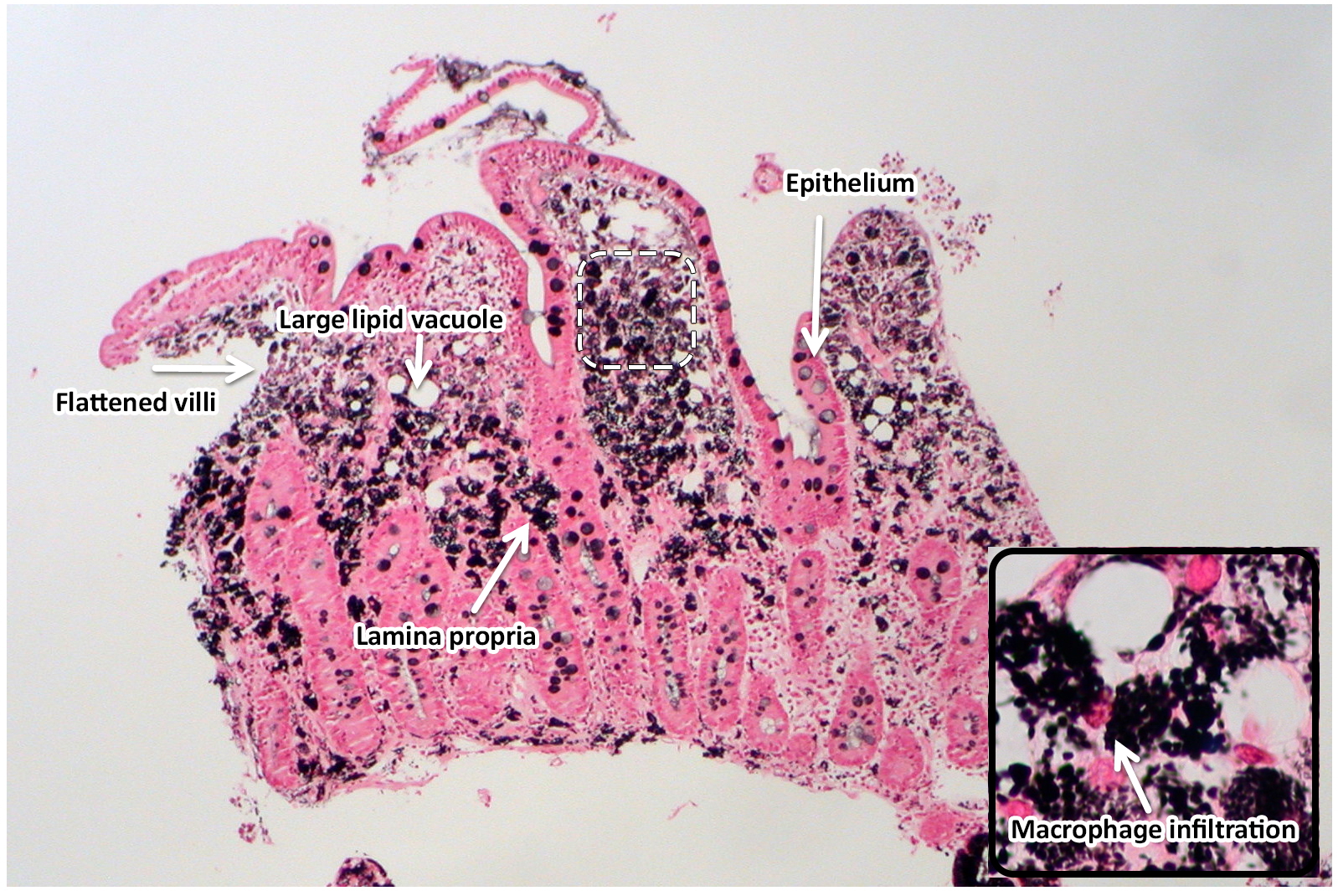
Biopsy
A biopsy of the small intestine is considered the gold standard for diagnosing this condition. During the procedure, a small tissue sample is taken from the lining of the intestine and examined under a microscope. The presence of foamy macrophages containing the bacterium confirms the diagnosis.
Polymerase Chain Reaction Testing
This advanced molecular technique detects the DNA of the bacterium in various samples, including blood, cerebrospinal fluid, or tissue. It is highly sensitive and specific, making it a valuable tool for confirming the diagnosis.
Treatment of Whipple’s Disease
Once diagnosed, prompt and appropriate treatment is essential to manage the condition effectively. The treatment approach typically involves a combination of antibiotics and supportive care to address symptoms and complications.
Antibiotic Therapy
Antibiotics are the cornerstone of treatment for this condition. The goal is to eradicate the bacterium from the body and prevent further damage. The treatment regimen usually includes:
- Initial Phase: A two-week course of intravenous antibiotics, such as ceftriaxone or penicillin, is administered to target the bacterium aggressively.
- Maintenance Phase: Following the initial phase, oral antibiotics like trimethoprim-sulfamethoxazole are prescribed for one to two years to ensure complete eradication of the infection.
Supportive Care
In addition to antibiotics, supportive care is crucial to manage symptoms and improve the patient’s quality of life. This may include:
- Nutritional Support: Patients with malnutrition may require dietary supplements or intravenous nutrition to restore nutrient levels.
- Pain Management: Medications to alleviate joint pain and other discomforts may be prescribed.
- Monitoring and Follow-Up: Regular follow-up appointments are necessary to monitor progress, adjust treatment, and address any complications.
Treatment of Neurological Involvement
If the disease affects the nervous system, additional treatments may be required. These could include:
- Extended Antibiotic Therapy: Longer courses of antibiotics may be necessary to penetrate the blood-brain barrier and eliminate the bacterium from the central nervous system.
- Neurological Rehabilitation: Physical therapy, occupational therapy, and other rehabilitation services can help patients regain lost functions and improve their quality of life.
Management of Cardiovascular Complications
In cases where the heart is involved, specialized care is needed. Treatment may involve:
- Antibiotics for Endocarditis: Specific antibiotic regimens are used to treat inflammation of the heart lining.
- Cardiac Monitoring: Regular echocardiograms and other tests may be conducted to assess heart function and detect any abnormalities.
Challenges in Managing Whipple’s Disease
Despite advances in medical science, managing this condition remains challenging. Several factors contribute to these difficulties:
Delayed Diagnosis
The nonspecific nature of the symptoms often leads to misdiagnosis or delayed diagnosis. By the time the correct diagnosis is made, significant damage may have already occurred.
Relapse Risk
Even with appropriate treatment, there is a risk of relapse. Patients must adhere strictly to their antibiotic regimen and attend regular follow-up appointments to minimize this risk.
Complexity of Treatment
The need for long-term antibiotic therapy and multidisciplinary care can be burdensome for patients. Managing side effects, ensuring compliance, and addressing complications require careful coordination among healthcare providers.
Raising Awareness and Improving Outcomes
Increasing awareness of this condition among healthcare professionals and the general public is vital for improving outcomes. Early recognition of symptoms, timely diagnosis, and appropriate treatment can significantly enhance the prognosis for affected individuals.
Research into the disease continues, with scientists exploring new diagnostic tools, treatment options, and preventive measures. Collaborative efforts between researchers, clinicians, and patient advocacy groups are essential to advance understanding and care for those living with this condition.