Granulomatosis with Polyangiitis, formerly known as Wegener’s Granulomatosis, is a rare autoimmune disorder that primarily affects the respiratory tract and kidneys. This condition is part of a group of diseases called vasculitis, which involves inflammation of blood vessels. In this article, we will explore the various aspects of this complex disease, including its causes, symptoms, diagnosis, treatment options, and ongoing research efforts.
Understanding the Disease
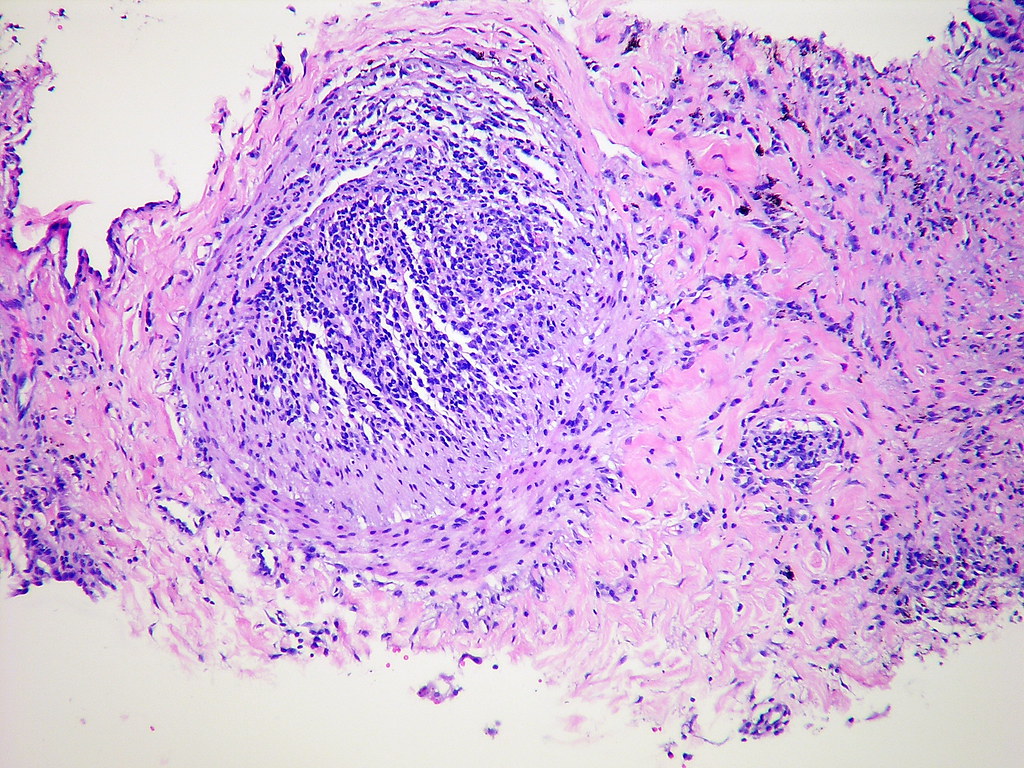
Granulomatosis with Polyangiitis is characterized by the formation of granulomas, which are small areas of inflammation, in affected tissues. The disease predominantly targets the upper respiratory tract, lungs, and kidneys but can also involve other organs such as the eyes, ears, skin, and nervous system. It is a systemic condition, meaning it can affect multiple parts of the body simultaneously.
Historical Background
- Discovery: The condition was first described in the 1930s by German pathologist Heinz Karl Ernst Wegener, after whom it was originally named.
- Name Change: In 2011, the name was officially changed to Granulomatosis with Polyangiitis to avoid any association with Wegener’s controversial past during World War II.
Causes and Risk Factors
The exact cause of this disease remains unknown, but researchers believe it results from a combination of genetic and environmental factors. Here are some key points to consider:
Genetic Predisposition
- Some individuals may have a genetic predisposition that makes them more susceptible to developing the condition.
- Certain gene variations have been associated with an increased risk, although no single gene has been identified as the sole cause.
Environmental Triggers
- Infections, particularly those involving bacteria or viruses, might trigger the immune system to malfunction in susceptible individuals.
- Exposure to certain chemicals or pollutants could also play a role in initiating the disease process.
Immune System Malfunction
At its core, this disease involves an abnormal response by the immune system. Instead of attacking harmful invaders like bacteria or viruses, the immune system mistakenly targets healthy tissues, leading to inflammation and damage.
Symptoms and Clinical Presentation
The symptoms of this condition can vary widely depending on which organs are affected. Early recognition of these symptoms is crucial for timely diagnosis and treatment.
Upper Respiratory Tract Symptoms
- Nasal congestion or frequent nosebleeds
- Sinus pain and infections
- Ear pain or hearing loss
Lung Symptoms
- Shortness of breath
- Coughing, sometimes with blood
- Chest pain
Kidney Symptoms
- Blood in urine
- Protein in urine
- Decreased kidney function
Other Possible Symptoms
- Fever and fatigue
- Joint pain and swelling
- Skin rashes or ulcers
- Eye problems such as redness, pain, or vision changes
Diagnosis
Diagnosing this condition can be challenging due to its varied symptoms and the fact that it mimics other diseases. A combination of clinical evaluation, laboratory tests, and imaging studies is typically required.
Clinical Evaluation
- A thorough medical history and physical examination are essential first steps.
- Doctors look for characteristic signs such as nasal crusting, sinus tenderness, or lung abnormalities.
Laboratory Tests
- Blood tests may reveal elevated markers of inflammation, such as C-reactive protein or erythrocyte sedimentation rate.
- Antineutrophil cytoplasmic antibodies, specifically the cytoplasmic pattern, are often present and serve as a diagnostic marker.
Imaging Studies
- Chest X-rays or CT scans can help identify lung involvement, such as nodules or cavities.
- Sinus imaging may show thickening or blockages indicative of chronic sinusitis.
Biopsy
- A tissue biopsy from affected areas, such as the lungs or kidneys, can confirm the presence of granulomas and vasculitis.
- This step is often necessary to rule out other conditions with similar presentations.
Treatment Options
While there is no cure for this condition, effective treatments are available to control symptoms, induce remission, and prevent relapses. Treatment plans are highly individualized based on the severity and extent of organ involvement.
Medications
- Corticosteroids: These powerful anti-inflammatory drugs are usually the first line of treatment to quickly reduce inflammation.
- Immunosuppressive Drugs: Medications like cyclophosphamide or rituximab are used to suppress the overactive immune response.
- Maintenance Therapy: Once remission is achieved, less potent immunosuppressants such as azathioprine or methotrexate may be prescribed to maintain remission.
Plasmapheresis
- In severe cases, particularly when kidney function is severely compromised, plasmapheresis may be used to remove harmful antibodies from the blood.
Supportive Care
- Pain management and physical therapy can help alleviate joint pain and improve mobility.
- Dietary adjustments and supplements may be recommended to support overall health and manage side effects of medications.
Ongoing Research and Future Directions
Research into this condition continues to advance, offering hope for improved treatments and outcomes. Some areas of focus include:
New Therapeutic Targets
- Scientists are exploring novel biological pathways that could be targeted by new medications to better control the immune response.
Genetic Studies
- Further investigation into genetic factors may lead to personalized treatment approaches tailored to an individual’s genetic makeup.
Long-term Outcomes
- Studies are underway to better understand the long-term effects of current treatments and to develop strategies to minimize side effects.
Living with the Condition
Managing this condition requires a comprehensive approach that includes medical treatment, lifestyle adjustments, and emotional support.
Lifestyle Modifications
- Adopting a healthy diet, regular exercise, and adequate rest can help bolster the immune system and improve overall well-being.
- Avoiding smoking and exposure to respiratory irritants is crucial to protect lung health.
Emotional and Psychological Support
- Living with a chronic illness can be emotionally taxing. Counseling or support groups can provide valuable coping strategies and a sense of community.
Regular Monitoring
- Frequent follow-ups with healthcare providers are essential to monitor disease activity and adjust treatment as needed.
- Patients should report any new or worsening symptoms promptly to their doctors.
Educational Resources and Advocacy
Raising awareness and providing education about this condition is vital for early diagnosis and effective management. Numerous organizations offer resources and support for patients and their families.
Support Organizations
- Groups like the Vasculitis Foundation provide educational materials, patient stories, and advocacy opportunities.
Research Participation
- Patients are encouraged to participate in clinical trials and research studies to contribute to scientific advancements and potentially benefit from cutting-edge treatments.