Vulvodynia, often abbreviated as VD, is a complex and often misunderstood condition that affects countless women worldwide. It refers to chronic pain or discomfort in the vulvar region without an identifiable cause. For many women, this condition can be both physically and emotionally challenging, leading to significant disruptions in daily life, relationships, and overall well-being. In this article, we will delve into the intricacies of this condition, exploring its symptoms, potential causes, diagnosis process, treatment options, and the impact it has on those who live with it.
What is Vulvodynia?
Vulvodynia is characterized by persistent pain in the area around the opening of the vagina, known as the vulva. The pain can vary in intensity and may be described as burning, stinging, rawness, or throbbing. This discomfort can occur spontaneously or be triggered by touch, pressure, or certain activities such as sitting, exercising, or sexual intercourse. Unlike other medical conditions, vulvodynia does not have a visible sign or a definitive diagnostic test, making it difficult for healthcare providers to identify and treat effectively.
Types of Vulvodynia
- Generalized Vulvodynia: Pain is felt across the entire vulvar area and can occur intermittently or constantly. It may be triggered by touch, pressure, or even without any apparent cause.
- Vulvar Vestibulitis Syndrome: Pain is localized to the vestibule, which is the area around the vaginal opening. This type of pain is often provoked by touch or pressure, such as during sexual intercourse or when inserting a tampon.
Symptoms of Vulvodynia
The symptoms of vulvodynia can differ from person to person, but some common experiences include:
- Burning or stinging sensations in the vulvar area
- Rawness or irritation that feels like the skin is being rubbed raw
- Pain during or after sexual intercourse
- Discomfort while sitting for prolonged periods
- Pain when wearing tight clothing or using sanitary products
It is important to note that the severity of these symptoms can fluctuate over time, and some individuals may experience periods of relief followed by flare-ups.
Potential Causes of Vulvodynia
Despite extensive research, the exact cause of vulvodynia remains unknown. However, several factors are believed to contribute to the development of this condition:
Hormonal Changes
Hormonal imbalances, particularly involving estrogen and testosterone, may play a role in vulvodynia. Fluctuations in hormone levels can affect the health of vulvar tissues, making them more sensitive or prone to irritation.
Nerve Damage or Irritation
Some researchers suggest that nerve damage or irritation in the vulvar region could lead to chronic pain. Conditions such as pudendal neuralgia, where the pudendal nerve becomes compressed or damaged, might contribute to vulvodynia symptoms.
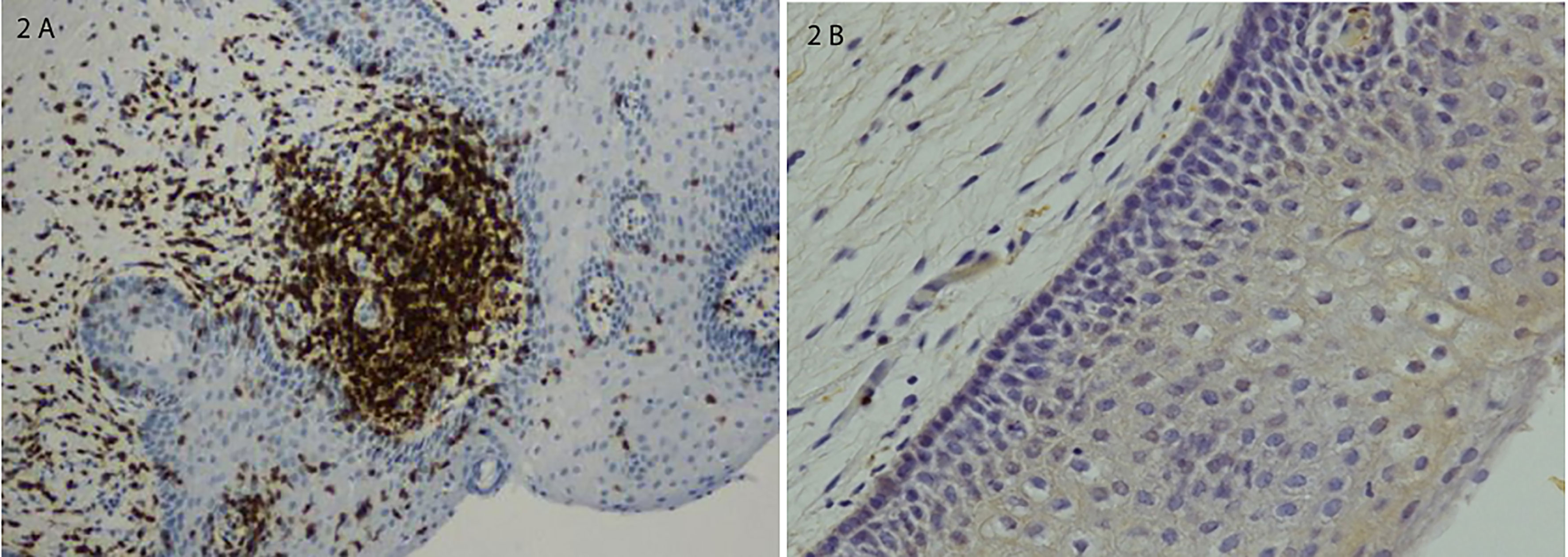
Inflammation and Immune System Response
Chronic inflammation or an overactive immune response may also be involved. Women with autoimmune disorders or allergies may be at a higher risk of developing vulvodynia due to heightened sensitivity in their bodies.
Muscle Tension and Pelvic Floor Dysfunction
Tightness or spasms in the pelvic floor muscles can exacerbate pain in the vulvar area. Pelvic floor dysfunction is often linked to stress, anxiety, or previous trauma, further complicating the condition.
Psychological Factors
While psychological factors do not directly cause vulvodynia, they can influence how individuals perceive and cope with pain. Stress, anxiety, and depression may worsen symptoms and make it harder to manage the condition effectively.
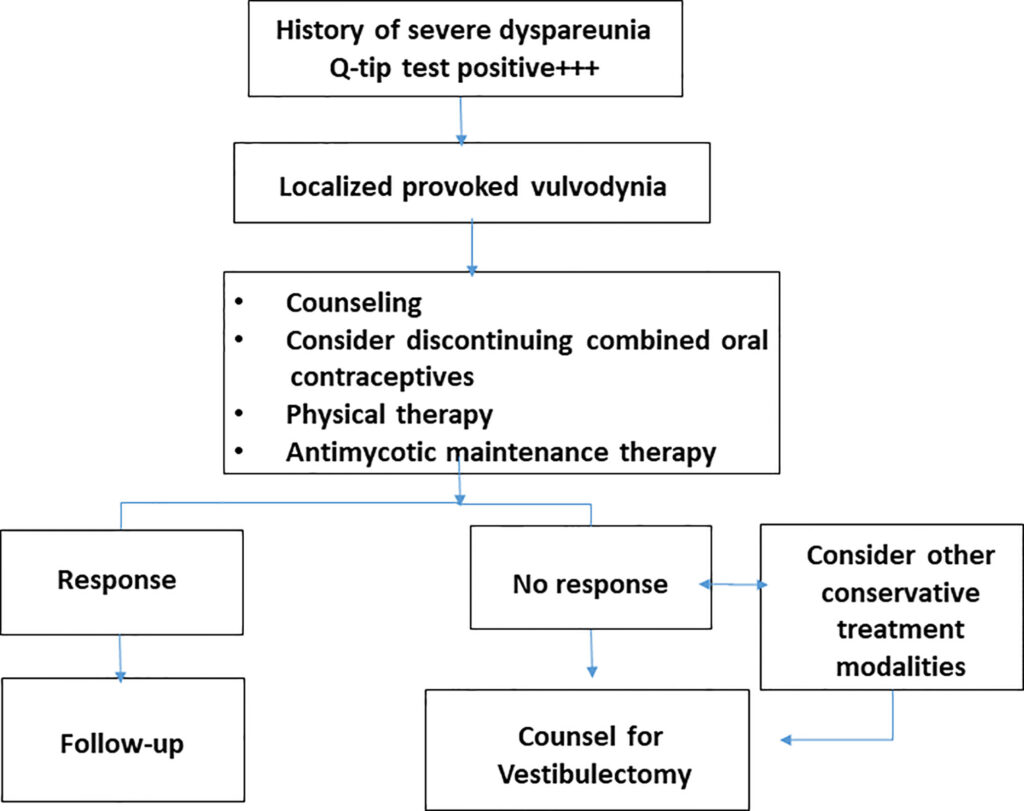
Diagnosing Vulvodynia
Diagnosing vulvodynia can be challenging because there are no specific tests to confirm its presence. Instead, healthcare providers rely on a combination of patient history, physical examination, and exclusion of other possible causes of vulvar pain.
Steps in Diagnosis
- Patient History: A detailed discussion about the nature, duration, and triggers of the pain helps doctors understand the pattern and severity of symptoms.
- Physical Examination: During the exam, the healthcare provider will carefully inspect the vulvar area for signs of infection, inflammation, or skin abnormalities. They may also apply gentle pressure to identify tender areas.
- Ruling Out Other Conditions: Tests such as cultures, biopsies, or imaging studies may be conducted to rule out infections, dermatological issues, or neurological disorders that could mimic vulvodynia.
Once other potential causes are excluded, a diagnosis of vulvodynia may be considered if the pain persists for at least three to six months.
Treatment Options for Vulvodynia
There is no one-size-fits-all treatment for vulvodynia, as each individual’s experience with the condition is unique. Treatment plans are typically tailored to address the specific symptoms and underlying factors contributing to the pain. Below are some common approaches:
Medications
- Topical Treatments: Prescription creams containing medications like lidocaine or capsaicin can help numb the area and reduce pain.
- Oral Medications: Antidepressants, anticonvulsants, or nerve pain medications may be prescribed to manage chronic pain and improve quality of life.
- Hormonal Therapies: For women whose symptoms are influenced by hormonal changes, topical estrogen therapy may provide relief.
Physical Therapy
Pelvic floor physical therapy focuses on relaxing and strengthening the muscles in the pelvic region. Techniques such as biofeedback, manual therapy, and relaxation exercises can help alleviate muscle tension and reduce pain.
Cognitive Behavioral Therapy
This form of therapy addresses the emotional and psychological aspects of living with chronic pain. By teaching coping strategies and reframing negative thought patterns, cognitive behavioral therapy can empower individuals to better manage their symptoms.
Lifestyle Modifications
Simple lifestyle changes can make a significant difference in managing vulvodynia:
- Avoiding irritants such as scented soaps, detergents, and tight clothing
- Using water-based lubricants during sexual activity
- Practicing stress-reduction techniques like yoga, meditation, or deep breathing
Surgical Interventions
In rare cases where conservative treatments fail, surgery may be considered. A procedure called vestibulectomy involves removing the affected tissue in the vestibule to relieve localized pain.
The Emotional and Social Impact of Vulvodynia
Living with vulvodynia extends beyond physical discomfort; it can profoundly affect mental health and social interactions. Many women report feelings of isolation, frustration, and embarrassment due to the intimate nature of the condition. Relationships, especially romantic ones, can become strained as a result of painful intercourse or fear of intimacy.
Support groups, both online and in-person, offer a safe space for individuals to share their experiences and connect with others facing similar challenges. Counseling or therapy can also help address the emotional toll of living with chronic pain and foster resilience.
Research and Future Directions
Ongoing research aims to uncover the root causes of vulvodynia and develop more effective treatments. Advances in understanding the role of genetics, neurobiology, and immune system interactions hold promise for breakthroughs in managing this condition. Additionally, increased awareness and education among healthcare providers can lead to earlier diagnoses and improved care for affected individuals.