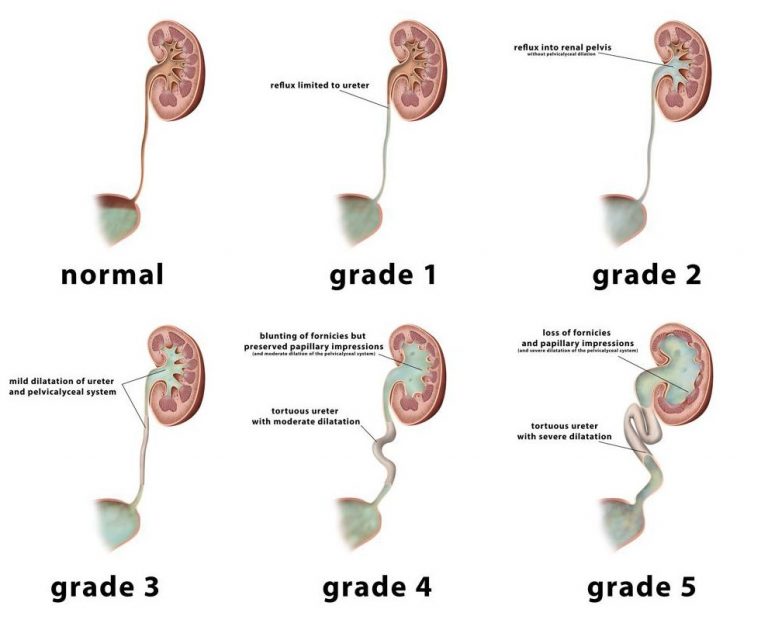
Vesicoureteral reflux, commonly abbreviated as VUR, is a condition that affects the urinary tract. It occurs when urine flows backward from the bladder into the ureters and sometimes even reaches the kidneys. This abnormal flow can lead to infections, kidney damage, and other complications if left untreated. Understanding this condition is crucial for early detection and effective management. In this article, we will explore the causes, symptoms, diagnosis methods, and treatment options available for vesicoureteral reflux.
What is Vesicoureteral Reflux?
Vesicoureteral reflux is a disorder in which urine flows in the wrong direction, moving from the bladder back up into the tubes that connect the kidneys to the bladder, known as the ureters. Normally, urine flows in one direction—from the kidneys to the bladder—and then exits the body through the urethra. However, in individuals with this condition, the valve-like mechanism at the junction of the ureters and bladder does not function properly, allowing urine to flow backward.
Types of Vesicoureteral Reflux
- Primary Vesicoureteral Reflux: This type is present at birth and occurs due to an abnormality in the development of the valve mechanism between the ureters and the bladder.
- Secondary Vesicoureteral Reflux: This form develops later in life and is often caused by factors such as urinary tract infections, blockages, or nerve problems affecting bladder function.
Causes of Vesicoureteral Reflux
The exact cause of vesicoureteral reflux depends on whether it is primary or secondary. Below are the common causes associated with each type:
Primary Vesicoureteral Reflux
- Congenital Defects: In many cases, children are born with a defect in the valve-like structure where the ureters meet the bladder. This structural issue prevents the valve from closing properly, allowing urine to flow back into the ureters.
- Genetic Factors: There is evidence suggesting that vesicoureteral reflux can run in families. If a parent or sibling has had this condition, there may be an increased risk for other family members.
Secondary Vesicoureteral Reflux
- Urinary Tract Infections: Severe or repeated infections of the urinary tract can damage the muscles and tissues around the bladder, leading to improper functioning of the valve mechanism.
- Bladder Outlet Obstruction: Conditions that cause a blockage in the bladder outlet, such as an enlarged prostate in men or certain congenital abnormalities, can increase pressure within the bladder and force urine to flow backward.
- Neurogenic Bladder: Disorders affecting the nerves that control bladder function, such as spinal cord injuries or diseases like multiple sclerosis, can disrupt normal bladder emptying and contribute to reflux.
Symptoms of Vesicoureteral Reflux
The symptoms of vesicoureteral reflux can vary depending on the severity of the condition and the age of the individual. Some people may not experience any noticeable symptoms, while others may have more pronounced signs. Common symptoms include:
- Recurrent Urinary Tract Infections: Frequent infections are one of the most common indicators of vesicoureteral reflux. These infections can cause symptoms such as pain during urination, frequent urge to urinate, and cloudy or foul-smelling urine.
- Fever: High fever without an obvious cause can sometimes signal a kidney infection resulting from untreated reflux.
- Pain in the Abdomen or Back: Individuals with vesicoureteral reflux may experience discomfort or pain in the lower abdomen or back, particularly if the condition has led to kidney involvement.
- Blood in the Urine: Hematuria, or the presence of blood in the urine, can occur due to irritation or damage to the urinary tract caused by backward urine flow.
- Poor Growth in Children: In severe cases, especially in young children, vesicoureteral reflux can interfere with proper nutrition and growth due to chronic illness or kidney dysfunction.
Diagnosis of Vesicoureteral Reflux
Diagnosing vesicoureteral reflux typically involves a combination of medical history evaluation, physical examination, and specialized tests. Early diagnosis is essential to prevent complications such as kidney scarring or permanent damage.
Medical History and Physical Examination
A healthcare provider will begin by reviewing the patient’s medical history, paying close attention to any recurring urinary tract infections, family history of similar conditions, and symptoms reported by the patient. A thorough physical examination may also reveal signs of infection or abnormalities in the urinary tract.
Specialized Tests
- Voiding Cystourethrogram (VCUG): This imaging test uses X-rays to visualize the bladder and ureters during urination. A contrast dye is inserted into the bladder through a catheter, allowing doctors to observe whether urine flows backward into the ureters.
- Renal Ultrasound: An ultrasound of the kidneys and bladder provides detailed images of these organs and helps identify structural abnormalities, swelling, or scarring.
- Nuclear Scan: Also known as a radionuclide cystogram, this test involves injecting a small amount of radioactive material into the bladder to track urine flow and assess kidney function.
- Urine Tests: Urinalysis and urine culture tests are performed to check for signs of infection, such as bacteria, white blood cells, or red blood cells in the urine.
Treatment Options for Vesicoureteral Reflux
The treatment approach for vesicoureteral reflux depends on several factors, including the severity of the condition, the age of the patient, and whether complications such as kidney damage have occurred. Treatment aims to prevent urinary tract infections, protect kidney function, and correct the underlying problem.
Conservative Management
In mild cases, especially in children, conservative management may be sufficient to manage the condition. This approach includes:
- Antibiotics: Low-dose antibiotics may be prescribed to prevent urinary tract infections and reduce the risk of kidney damage.
- Regular Monitoring: Patients are closely monitored through periodic follow-up visits and tests to ensure that the condition does not worsen over time.
Surgical Intervention
If conservative measures fail or if the condition is severe, surgical intervention may be necessary. Surgical procedures aim to correct the defective valve mechanism and restore normal urine flow. Common surgical techniques include:
- Endoscopic Injection: A minimally invasive procedure in which a bulking agent is injected near the opening of the ureter to strengthen the valve and prevent backward urine flow.
- Ureteral Reimplantation Surgery: This open surgery involves repositioning the ureters into the bladder wall to create a stronger valve mechanism. It is typically reserved for more severe cases or when endoscopic treatment is not effective.
Lifestyle Modifications
In addition to medical and surgical treatments, certain lifestyle changes can help manage vesicoureteral reflux and reduce the risk of complications:
- Hydration: Drinking plenty of water helps flush out bacteria from the urinary tract and reduces the likelihood of infections.
- Healthy Hygiene Practices: Proper hygiene, particularly in children, can minimize the risk of urinary tract infections.
- Avoiding Constipation: Maintaining regular bowel movements can alleviate pressure on the bladder and improve overall urinary health.
When to Seek Medical Attention
It is important to seek medical attention if you or your child experiences symptoms suggestive of vesicoureteral reflux. Prompt diagnosis and treatment can prevent serious complications such as kidney scarring, hypertension, or chronic kidney disease. Pay particular attention to recurrent urinary tract infections, persistent fever, or unexplained abdominal pain, as these could indicate an underlying issue requiring immediate care.
Living with Vesicoureteral Reflux
For many individuals, living with vesicoureteral reflux involves ongoing management and vigilance. Regular check-ups with a healthcare provider, adherence to prescribed treatments, and adopting healthy habits can significantly improve quality of life and reduce the risk of long-term complications. By staying informed and proactive, patients can effectively navigate the challenges posed by this condition.