Ventricular tachycardia, often abbreviated as VT, is a serious heart condition characterized by an abnormally rapid heartbeat originating in the ventricles, the lower chambers of the heart. This condition can disrupt the normal rhythm of the heart and may lead to life-threatening complications if not promptly addressed. In this article, we will explore the causes, symptoms, diagnostic methods, and treatment options for ventricular tachycardia.

What Is Ventricular Tachycardia?
Ventricular tachycardia occurs when the electrical signals that regulate the heartbeat become abnormal, causing the ventricles to beat faster than usual. A normal resting heart rate ranges between sixty and one hundred beats per minute. However, during an episode of ventricular tachycardia, the heart rate can exceed one hundred beats per minute, sometimes reaching up to two hundred or more. This rapid heartbeat prevents the heart from efficiently pumping blood to the rest of the body, which can result in dizziness, fainting, or even cardiac arrest in severe cases.
Types of Ventricular Tachycardia
- Sustained Ventricular Tachycardia: This type lasts for more than thirty seconds or requires medical intervention to stop. It is considered more dangerous because it can lead to complications such as heart failure or sudden cardiac death.
- Non-Sustained Ventricular Tachycardia: This type lasts for less than thirty seconds and often resolves on its own. While it may not always cause immediate harm, it can still be a warning sign of underlying heart issues.
Causes of Ventricular Tachycardia
The primary cause of ventricular tachycardia is an abnormality in the heart’s electrical system. Several factors can contribute to this condition, including:
Structural Heart Disease
One of the most common causes of ventricular tachycardia is structural damage to the heart. Conditions such as coronary artery disease, heart attacks, cardiomyopathy, and heart valve disorders can scar the heart tissue, disrupting the normal flow of electrical signals.
Electrolyte Imbalances
Electrolytes such as potassium, sodium, calcium, and magnesium play a crucial role in maintaining the heart’s electrical activity. An imbalance in these electrolytes, whether due to dehydration, kidney disease, or certain medications, can trigger episodes of ventricular tachycardia.
Medications and Substances
Certain medications, particularly those used to treat heart conditions, can inadvertently cause ventricular tachycardia as a side effect. Additionally, stimulants like cocaine and amphetamines can overstimulate the heart, leading to abnormal rhythms.
Genetic Factors
In some cases, ventricular tachycardia may be linked to inherited conditions such as long QT syndrome or Brugada syndrome. These genetic disorders affect the heart’s electrical system and increase the risk of arrhythmias.
Other Contributing Factors
- High blood pressure
- Chronic alcohol abuse
- Severe infections or inflammation of the heart
- Excessive caffeine consumption
Symptoms of Ventricular Tachycardia
The symptoms of ventricular tachycardia can vary depending on the duration and severity of the episode. Some individuals may experience mild symptoms, while others may face life-threatening complications. Common symptoms include:
Palpitations
A sensation of rapid, fluttering, or pounding heartbeats is one of the hallmark symptoms of ventricular tachycardia. This feeling may occur suddenly and can be alarming for the individual experiencing it.
Dizziness and Lightheadedness
Due to the heart’s inability to pump blood effectively during an episode, individuals may feel dizzy or lightheaded. In some cases, this can progress to fainting, also known as syncope.
Chest Pain
Chest pain or discomfort is another common symptom of ventricular tachycardia. This pain may feel like pressure, tightness, or squeezing in the chest and should not be ignored, as it could indicate a more serious underlying issue.
Shortness of Breath
As the heart struggles to maintain adequate blood flow, individuals may experience shortness of breath, even during minimal physical activity or at rest.
Fatigue
Feeling unusually tired or weak is another potential symptom of ventricular tachycardia. This fatigue is often due to the reduced efficiency of the heart in delivering oxygen-rich blood to the body’s tissues.
Diagnosis of Ventricular Tachycardia
Diagnosing ventricular tachycardia typically involves a combination of medical history evaluation, physical examination, and specialized tests. Early and accurate diagnosis is critical for effective management of the condition.
Medical History and Physical Examination
A healthcare provider will begin by reviewing the patient’s medical history, including any previous heart conditions, family history of heart disease, and lifestyle factors such as smoking or alcohol use. During the physical examination, the provider will listen to the heart and check for signs of irregular rhythms or other abnormalities.
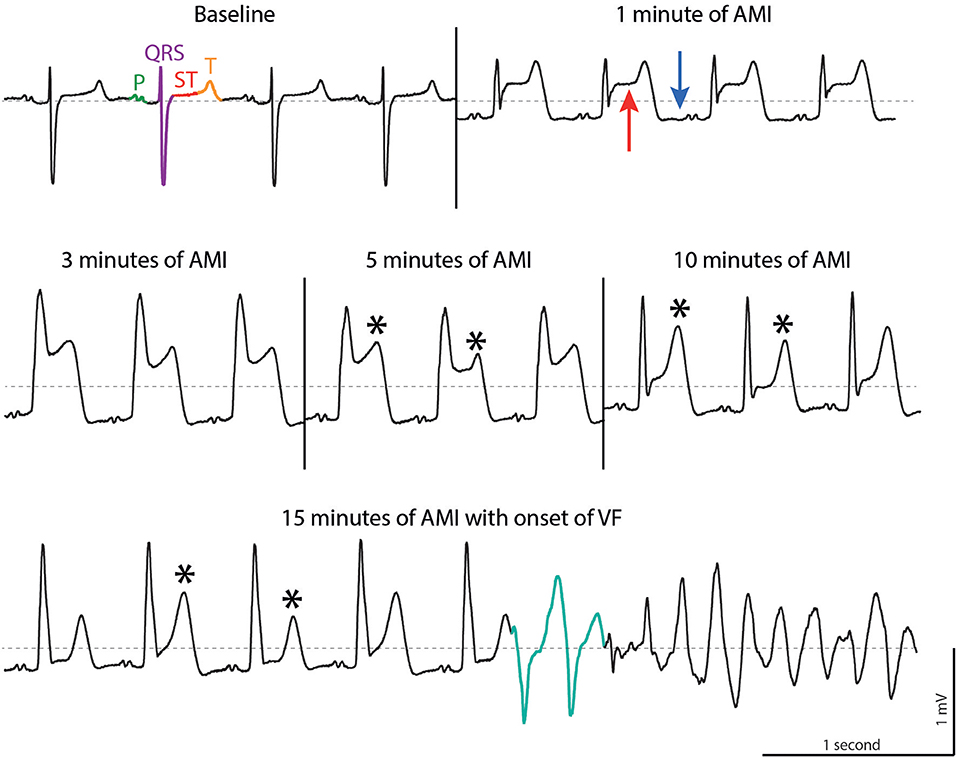
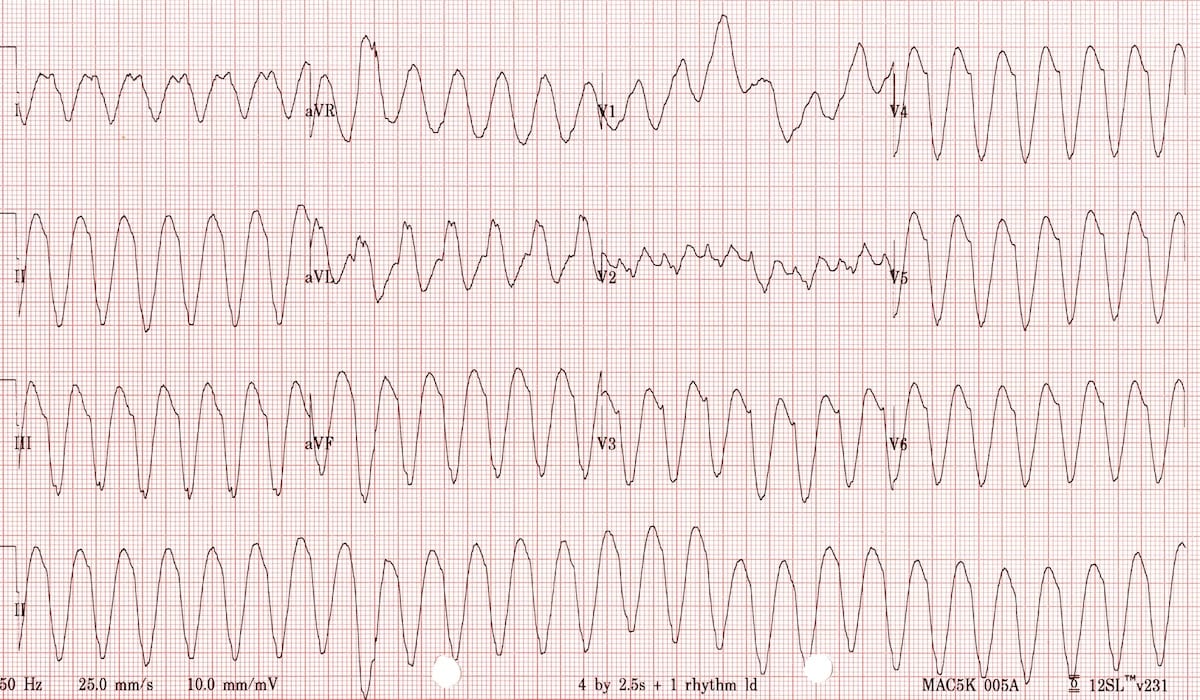
Electrocardiogram
An electrocardiogram, commonly referred to as an ECG, is one of the primary tools used to diagnose ventricular tachycardia. This non-invasive test records the electrical activity of the heart and can identify abnormal rhythms, including those associated with ventricular tachycardia.
Holter Monitor
For individuals who experience intermittent symptoms, a Holter monitor may be used. This portable device records the heart’s activity over a twenty-four to forty-eight-hour period, allowing healthcare providers to detect arrhythmias that may not occur during a standard ECG.
Event Monitor
Similar to a Holter monitor, an event monitor is used to track heart activity over a longer period, often several weeks. Patients activate the device when they experience symptoms, providing valuable data for diagnosis.
Echocardiogram
An echocardiogram uses sound waves to create detailed images of the heart’s structure and function. This test can help identify structural abnormalities or damage that may be contributing to ventricular tachycardia.
Electrophysiological Study
In some cases, an electrophysiological study may be performed. During this invasive procedure, thin wires are inserted into the heart to map its electrical activity and pinpoint the source of the abnormal rhythm.
Treatment Options for Ventricular Tachycardia
The treatment of ventricular tachycardia depends on the underlying cause, the severity of the condition, and the patient’s overall health. The primary goals of treatment are to restore a normal heart rhythm, prevent future episodes, and reduce the risk of complications.
Lifestyle Modifications
Making certain lifestyle changes can help manage ventricular tachycardia and reduce the risk of recurrence. These changes may include:
- Quitting smoking
- Limiting alcohol and caffeine intake
- Maintaining a healthy weight through diet and exercise
- Managing stress through relaxation techniques or therapy
Medications
Several types of medications can be used to treat ventricular tachycardia, including:
- Antiarrhythmic drugs to help regulate the heart’s rhythm
- Beta-blockers to slow the heart rate and reduce the workload on the heart
- Calcium channel blockers to control electrical activity in the heart
Implantable Cardioverter-Defibrillator
For individuals at high risk of life-threatening arrhythmias, an implantable cardioverter-defibrillator may be recommended. This small device is surgically implanted under the skin and continuously monitors the heart’s rhythm. If an abnormal rhythm is detected, the device delivers an electrical shock to restore a normal rhythm.
Catheter Ablation
Catheter ablation is a minimally invasive procedure used to treat ventricular tachycardia. During the procedure, thin catheters are inserted into the heart to locate and destroy the tissue responsible for the abnormal electrical signals.
Surgery
In rare cases, surgery may be necessary to address structural issues in the heart that are causing ventricular tachycardia. This may involve repairing damaged heart tissue or correcting congenital defects.
Emergency Treatment
If ventricular tachycardia leads to cardiac arrest, immediate emergency treatment is required. This may include cardiopulmonary resuscitation and the use of a defibrillator to restore a normal heart rhythm.