A Ventricular Septal Defect, commonly referred to as VSD, is a congenital heart condition that affects infants and sometimes adults. It involves an abnormal opening in the wall that separates the two lower chambers of the heart, known as the ventricles. This defect allows oxygen-rich blood to mix with oxygen-poor blood, which can lead to various complications if not addressed properly. In this article, we will explore what this condition entails, its causes, symptoms, and how it can be managed or treated.

What Is a Hole in the Heart?
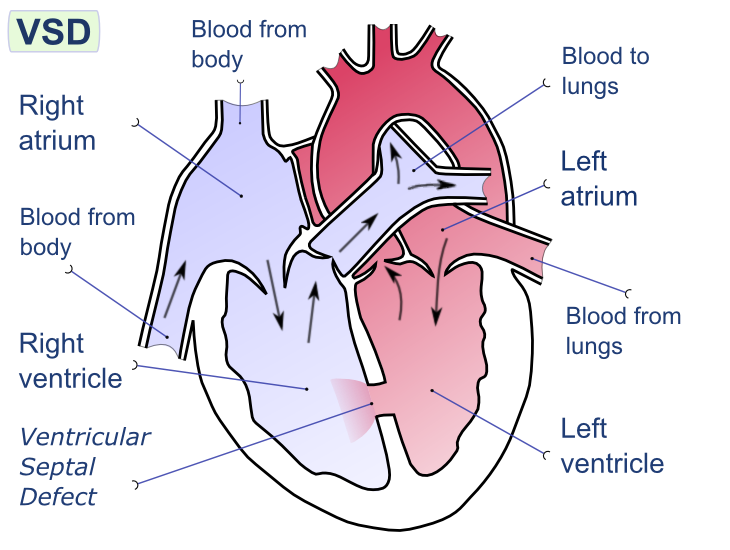
A hole in the heart refers to an opening in the septum, the muscular wall that divides the left and right sides of the heart. When this hole occurs between the two lower chambers, or ventricles, it is called a ventricular septal defect. Normally, the septum ensures that oxygen-rich blood from the lungs does not mix with oxygen-poor blood returning from the body. However, when a hole is present, blood flows through the opening, disrupting the normal flow of blood and potentially overworking the heart and lungs.
This condition is one of the most common types of congenital heart defects, meaning it is present at birth. While some small holes may close on their own over time, larger ones often require medical intervention to prevent long-term complications.
How Does a Hole in the Heart Develop?
The exact cause of a hole in the heart is not always clear, but several factors are believed to contribute to its development. These include:
- Genetic Factors: Some cases are linked to inherited genetic conditions or chromosomal abnormalities, such as Down syndrome.
- Environmental Influences: Exposure to certain substances during pregnancy, such as alcohol, tobacco, or specific medications, may increase the risk of heart defects in the developing fetus.
- Infections During Pregnancy: Maternal infections like rubella (German measles) can interfere with the normal development of the fetal heart.
- Nutritional Deficiencies: A lack of essential nutrients, particularly folic acid, during early pregnancy has been associated with an increased risk of congenital heart defects.
While these factors can raise the likelihood of a hole in the heart, many cases occur without any identifiable cause. Researchers continue to study the complex interplay of genetics and environmental influences to better understand why these defects develop.
Signs and Symptoms of a Hole in the Heart
The symptoms of a hole in the heart can vary depending on the size of the defect and the age of the individual. In some cases, especially when the hole is small, there may be no noticeable symptoms at all. However, larger holes or those that persist into adulthood often lead to more pronounced signs. Common symptoms include:
- Rapid Breathing: Infants with a significant hole in the heart may breathe faster than usual, even when they are resting.
- Poor Weight Gain: Babies may struggle to gain weight because their bodies are working harder to compensate for the inefficient blood flow.
- Fatigue: Children and adults with this condition may tire easily during physical activities due to reduced oxygen levels in the blood.
- Frequent Respiratory Infections: The increased blood flow to the lungs caused by the defect can make individuals more susceptible to infections like pneumonia.
- Heart Murmur: A distinctive sound heard through a stethoscope, often described as a “whooshing” noise, is a common indicator of abnormal blood flow.
In severe cases, untreated holes in the heart can lead to complications such as pulmonary hypertension (high blood pressure in the lungs), heart failure, or developmental delays in children.
Diagnosing a Hole in the Heart
Early diagnosis is crucial for managing a hole in the heart effectively. Healthcare providers typically use a combination of methods to confirm the presence and severity of the defect:
Physical Examination
During a routine checkup, a doctor may detect a heart murmur, which prompts further investigation. While not all murmurs indicate a serious problem, they are often the first clue that something might be amiss.
Echocardiogram
An echocardiogram is a non-invasive imaging test that uses sound waves to create detailed pictures of the heart. This test allows doctors to see the size and location of the hole, as well as assess how it affects blood flow.
Chest X-Ray
A chest X-ray provides images of the heart and lungs, helping to identify any enlargement of the heart or other abnormalities related to the defect.
Electrocardiogram (ECG)
An electrocardiogram measures the electrical activity of the heart and can reveal irregularities in heart rhythm or structure that may suggest the presence of a hole.
Cardiac Catheterization
In some cases, a more invasive procedure called cardiac catheterization may be necessary. This involves inserting a thin tube into a blood vessel and guiding it to the heart to gather detailed information about the defect.
Treatment Options for a Hole in the Heart
The treatment approach depends on the size of the hole, the severity of symptoms, and the age of the patient. In mild cases, regular monitoring may be sufficient, while more serious defects often require intervention.
Observation and Monitoring
Small holes that do not cause symptoms or complications may close naturally over time, particularly in infants. Regular follow-up appointments with a pediatric cardiologist are essential to ensure the defect resolves without causing harm.
Medications
While medications cannot close a hole in the heart, they can help manage symptoms and reduce the risk of complications. For example:
- Diuretics: These drugs help remove excess fluid from the body, easing the workload on the heart.
- Beta-Blockers: These medications slow the heart rate and lower blood pressure, reducing strain on the heart.
Surgical Repair
For larger holes or those that fail to close on their own, surgery may be necessary. There are two primary surgical approaches:
- Open-Heart Surgery: This procedure involves making an incision in the chest to access the heart directly. The surgeon patches the hole using synthetic material or tissue from another part of the body.
- Catheter-Based Procedures: A less invasive option, this technique involves threading a catheter through a blood vessel to the heart. A specially designed device is then used to plug the hole.
Both methods have high success rates, and most patients experience significant improvement after the procedure.
Lifestyle and Care Considerations
Living with a hole in the heart requires ongoing care and attention, even after successful treatment. Here are some important considerations:
Regular Checkups
Individuals who have undergone repair should continue seeing a cardiologist periodically to monitor their heart health and address any new concerns.
Healthy Diet and Exercise
Maintaining a balanced diet and engaging in regular physical activity can support overall cardiovascular health. However, it’s important to consult with a healthcare provider before starting any exercise program, especially for those with residual effects from the defect.
Preventing Infections
People with a history of heart defects may be at higher risk for endocarditis, an infection of the heart lining. Taking precautions, such as practicing good oral hygiene and informing dentists or surgeons about the condition, can help minimize this risk.
Emotional and Psychological Support
Managing a chronic condition like a hole in the heart can take an emotional toll on both patients and their families. Seeking support from counselors, support groups, or online communities can provide valuable coping strategies and encouragement.
Final Thoughts
A hole in the heart is a manageable condition with proper care and treatment. Advances in medical technology and surgical techniques have significantly improved outcomes for affected individuals. By staying informed and working closely with healthcare providers, patients can lead healthy, fulfilling lives despite this congenital challenge.