Uveitis, often abbreviated as UI, is a complex and potentially serious condition that affects the middle layer of the eye, known as the uvea. This inflammation can lead to discomfort, vision problems, and even permanent damage if not treated promptly. Understanding what this condition entails, its causes, symptoms, and treatment options is crucial for maintaining eye health. In this guide, we will delve into all aspects of this condition to provide you with a comprehensive overview.
What Is Uveitis?
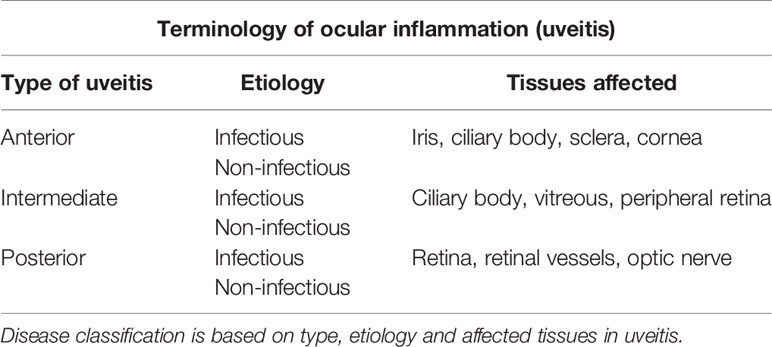
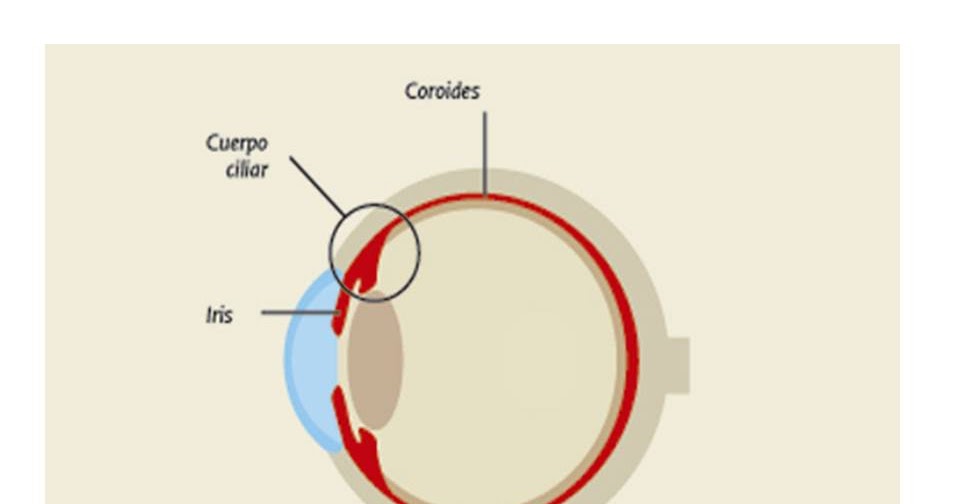
Uveitis refers to the inflammation of the uvea, which is the pigmented layer of the eye located between the inner retina and the outer fibrous layer composed of the sclera and cornea. The uvea consists of three main parts: the iris, the ciliary body, and the choroid. When any of these parts become inflamed, it can result in uveitis.
This condition can occur in people of all ages but is most commonly seen in individuals between the ages of twenty and sixty. It can affect one or both eyes and may develop suddenly or gradually over time. Without proper care, uveitis can lead to complications such as glaucoma, cataracts, or retinal damage.
Types of Uveitis
- Anterior Uveitis: This type affects the front part of the eye, specifically the iris. It is also sometimes referred to as iritis and is the most common form of the condition.
- Intermediate Uveitis: This form primarily involves the area just behind the ciliary body and can extend to the vitreous humor, the gel-like substance that fills the eye.
- Posterior Uveitis: This type affects the back part of the eye, including the retina and the choroid. It is often more severe and can cause significant vision loss.
- Panuveitis: This occurs when all layers of the uvea are inflamed. It is considered the most serious form of the condition due to its widespread impact on the eye.
Causes of Uveitis
The exact cause of uveitis is not always clear, but several factors can contribute to its development. These include:
Infections
Infectious agents such as bacteria, viruses, fungi, and parasites can trigger inflammation in the eye. Common infections associated with uveitis include herpes simplex, tuberculosis, syphilis, and toxoplasmosis.
Autoimmune Disorders
Autoimmune diseases occur when the immune system mistakenly attacks healthy tissues. Conditions like rheumatoid arthritis, lupus, and sarcoidosis can increase the risk of developing uveitis. In these cases, the immune response targets the eye, leading to inflammation.
Trauma or Injury
Physical trauma to the eye, whether from an accident or surgery, can cause inflammation. Even minor injuries can sometimes result in uveitis if the eye’s delicate structures are affected.
Other Factors
Some forms of uveitis have no identifiable cause and are classified as idiopathic. Additionally, certain medications and systemic illnesses, such as inflammatory bowel disease or multiple sclerosis, may also be linked to the development of uveitis.
Symptoms of Uveitis
The symptoms of uveitis can vary depending on the type and severity of the condition. However, some common signs to watch out for include:
- Eye redness
- Pain or discomfort in the eye
- Blurred or decreased vision
- Sensitivity to light
- Floating spots or specks in your field of vision
- Small pupil size or irregularly shaped pupil
If you experience any of these symptoms, especially if they persist or worsen, it is essential to seek medical attention promptly. Early diagnosis and treatment can help prevent complications and preserve your vision.
Diagnosing Uveitis
To diagnose uveitis, an eye care professional will perform a thorough examination of the eye. This process typically includes:
Medical History Review
Your doctor will ask about your symptoms, how long you have been experiencing them, and any underlying health conditions you may have. They will also inquire about recent injuries, surgeries, or infections that could be contributing factors.
Eye Examination
A comprehensive eye exam is crucial for identifying signs of inflammation. Your doctor may use specialized instruments to examine the front and back of your eye. They may also check your visual acuity and measure the pressure inside your eye to rule out other conditions like glaucoma.
Additional Tests
In some cases, additional tests may be necessary to determine the underlying cause of uveitis. These tests might include blood work, imaging studies like an MRI or CT scan, or a procedure called a fluorescein angiography, which uses dye to highlight blood vessels in the retina.
Treatment Options for Uveitis
The primary goal of treating uveitis is to reduce inflammation, relieve symptoms, and prevent complications. Treatment plans are tailored to the specific type and severity of the condition, as well as the underlying cause if known. Common treatment options include:
Medications
Anti-inflammatory medications, such as corticosteroids, are often prescribed to reduce swelling and irritation. These can be administered in the form of eye drops, injections, or oral pills, depending on the location and extent of the inflammation.
In cases where uveitis is caused by an infection, antibiotics, antiviral drugs, or antifungal medications may be used to target the infectious agent. For patients with autoimmune-related uveitis, immunosuppressive drugs may be recommended to control the immune response.
Surgical Interventions
In severe cases, surgical procedures may be necessary to address complications or deliver medication directly to the eye. One such procedure is a vitrectomy, which involves removing the vitreous humor to eliminate debris or scar tissue that may be affecting vision.
Lifestyle Adjustments
While medical treatments are essential, certain lifestyle changes can also support recovery and reduce the risk of recurrence. These include wearing sunglasses to protect the eyes from bright light, avoiding activities that strain the eyes, and managing stress through relaxation techniques.
Living with Uveitis
Managing uveitis requires ongoing care and vigilance. Regular follow-up appointments with your eye care provider are crucial to monitor the condition and adjust treatment as needed. Patients should also be aware of potential side effects from medications and report any concerns to their doctor immediately.
Education plays a vital role in living with uveitis. Understanding the condition, recognizing early warning signs, and adhering to prescribed treatments can significantly improve outcomes. Support groups and resources are available for individuals seeking guidance and encouragement from others who share similar experiences.
Preventing Uveitis
While it may not always be possible to prevent uveitis, there are steps you can take to reduce your risk:
- Maintain good overall health by eating a balanced diet, exercising regularly, and getting enough sleep.
- Protect your eyes from injury by wearing protective eyewear during sports or hazardous activities.
- Stay up-to-date with vaccinations to prevent infections that could lead to uveitis.
- Manage chronic health conditions, such as diabetes or autoimmune disorders, effectively to minimize complications.
By taking proactive measures and staying informed, you can safeguard your eye health and reduce the likelihood of developing uveitis.