Thrombophlebitis, commonly abbreviated as TP, refers to the inflammation of veins caused by the formation of blood clots. This condition can occur in both superficial and deep veins and may lead to serious complications if not treated promptly. Understanding its causes, types, symptoms, and treatment options is essential for managing this condition effectively.

Overview of Thrombophlebitis
Thrombophlebitis occurs when a vein becomes inflamed due to the presence of a blood clot. The inflammation can cause pain, swelling, and redness along the affected vein. This condition often develops in the legs but can also occur in other parts of the body. While superficial thrombophlebitis is generally less severe, deep vein thrombosis, which involves deeper veins, poses a higher risk of complications such as pulmonary embolism.
How Blood Clots Form
Blood clots are a natural part of the body’s healing process. When a blood vessel is injured, platelets and proteins in the blood work together to form a clot to stop the bleeding. However, when clots form without an injury or fail to dissolve after serving their purpose, they can block blood flow and cause inflammation. This abnormal clot formation is the primary cause of thrombophlebitis.
Types of Thrombophlebitis
Thrombophlebitis can be classified into two main types based on the location and depth of the affected veins:
Superficial Thrombophlebitis
- This type affects veins close to the surface of the skin.
- It is often associated with varicose veins or intravenous catheters.
- Symptoms include localized pain, tenderness, redness, and warmth over the affected area.
- While generally less dangerous, it can sometimes progress to deeper veins if left untreated.
Deep Vein Thrombosis
- This type involves veins located deep within the muscles, usually in the legs.
- It is more serious than superficial thrombophlebitis because the clots can break loose and travel to the lungs, causing a life-threatening condition known as pulmonary embolism.
- Symptoms may include swelling, pain, and a feeling of heaviness in the affected limb.
- In some cases, deep vein thrombosis may not present noticeable symptoms until complications arise.
Causes of Thrombophlebitis
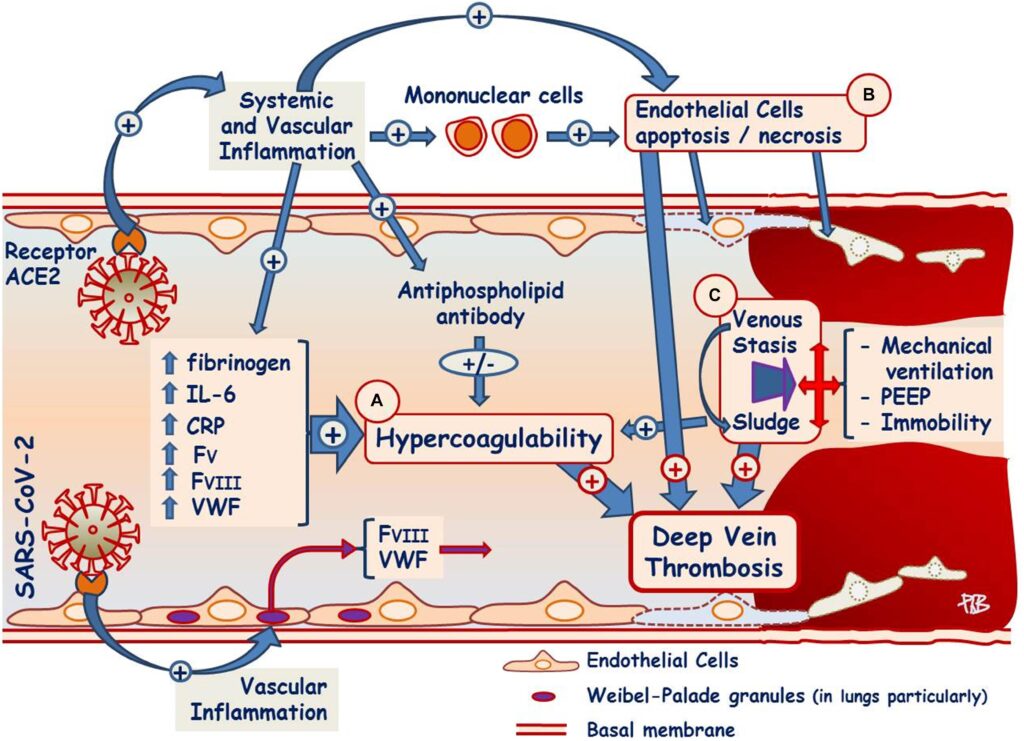
The development of thrombophlebitis is influenced by various factors that increase the likelihood of blood clot formation. These factors can be categorized into three main groups: venous stasis, hypercoagulability, and endothelial injury.
Venous Stasis
Venous stasis refers to the slowing or stagnation of blood flow within the veins. This can occur due to:
- Prolonged immobility, such as during long flights or bed rest after surgery.
- Obesity, which puts additional pressure on the veins in the legs.
- Varicose veins, which impair normal blood flow.
Hypercoagulability
Hypercoagulability refers to an increased tendency of the blood to clot. This can result from:
- Genetic disorders, such as Factor V Leiden mutation.
- Certain medications, including oral contraceptives and hormone replacement therapy.
- Medical conditions like cancer, inflammatory diseases, and pregnancy.
Endothelial Injury
Endothelial injury refers to damage to the inner lining of the veins. This can be caused by:
- Trauma or injury to the affected area.
- Insertion of intravenous catheters or needles.
- Chronic inflammatory conditions affecting the veins.
Risk Factors for Thrombophlebitis
Certain individuals are at a higher risk of developing thrombophlebitis due to specific predisposing factors. These include:
- Age: Older adults are more prone to blood clot formation.
- History of blood clots: Individuals who have experienced thrombophlebitis or deep vein thrombosis in the past are at greater risk.
- Smoking: Smoking damages blood vessels and increases clotting tendencies.
- Surgery or hospitalization: Prolonged periods of inactivity during recovery can lead to venous stasis.
- Underlying medical conditions: Conditions such as heart failure, diabetes, and autoimmune disorders elevate the risk.
Symptoms of Thrombophlebitis
The symptoms of thrombophlebitis vary depending on whether the condition affects superficial or deep veins. Common signs include:
- Pain or tenderness along the affected vein.
- Redness or discoloration of the skin over the vein.
- Swelling in the affected limb.
- A palpable cord-like structure beneath the skin in cases of superficial thrombophlebitis.
- Fever, although this is rare and typically indicates infection.
Diagnosis of Thrombophlebitis
Accurate diagnosis of thrombophlebitis is crucial for determining the appropriate treatment plan. Healthcare providers use several methods to diagnose this condition:
Physical Examination
A healthcare provider will examine the affected area for signs of inflammation, such as redness, warmth, and swelling. They may also check for a palpable cord-like vein in cases of superficial thrombophlebitis.
Ultrasound Imaging
An ultrasound is often used to visualize the veins and detect the presence of blood clots. This non-invasive test helps differentiate between superficial and deep vein involvement.
Blood Tests
Blood tests, such as D-dimer testing, may be performed to assess the likelihood of blood clot formation. Elevated levels of D-dimer indicate the presence of clot breakdown products in the blood.
Treatment Options for Thrombophlebitis
The treatment of thrombophlebitis depends on the type and severity of the condition. The primary goals of treatment are to reduce inflammation, prevent clot extension, and minimize the risk of complications.
Treatment for Superficial Thrombophlebitis
Superficial thrombophlebitis is typically managed with conservative measures:
- Warm Compresses: Applying warm compresses to the affected area can help alleviate pain and reduce inflammation.
- Compression Stockings: Wearing compression stockings improves blood flow and reduces swelling.
- Pain Relievers: Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can provide relief from discomfort.
- Elevation: Elevating the affected limb above heart level helps reduce swelling and promotes blood flow.
Treatment for Deep Vein Thrombosis
Deep vein thrombosis requires more aggressive treatment to prevent complications:
- Anticoagulant Medications: Blood thinners, such as heparin or warfarin, are prescribed to prevent the clot from growing and reduce the risk of new clots forming.
- Thrombolytic Therapy: In severe cases, medications that dissolve clots may be administered directly into the vein.
- Compression Devices: Intermittent pneumatic compression devices are used to improve circulation and prevent clot formation.
- Surgical Intervention: In rare cases, surgical removal of the clot or placement of a filter in the vena cava may be necessary to prevent pulmonary embolism.
Prevention of Thrombophlebitis
Preventing thrombophlebitis involves addressing modifiable risk factors and adopting healthy lifestyle practices:
- Stay Active: Regular physical activity promotes healthy blood flow and reduces the risk of venous stasis.
- Maintain a Healthy Weight: Losing excess weight alleviates pressure on the veins in the legs.
- Avoid Prolonged Immobility: If sitting for long periods, take breaks to stretch and move around.
- Quit Smoking: Smoking cessation improves overall vascular health.
- Use Compression Stockings: Individuals at high risk, such as those with a history of blood clots, should consider wearing compression stockings.
Complications of Untreated Thrombophlebitis
If left untreated, thrombophlebitis can lead to serious complications, particularly in cases of deep vein thrombosis. These complications include:
- Pulmonary Embolism: A blood clot that travels to the lungs can block blood flow and cause life-threatening respiratory distress.
- Post-Thrombotic Syndrome: Damage to the veins can result in chronic pain, swelling, and skin changes in the affected limb.
- Recurrent Blood Clots: Individuals with a history of thrombophlebitis are at higher risk of developing future clots.
When to Seek Medical Attention
It is important to seek medical attention if you experience any of the following symptoms:
- Sudden onset of severe pain or swelling in the leg.
- Shortness of breath, chest pain, or coughing up blood, which may indicate a pulmonary embolism.
- Signs of infection, such as fever or pus drainage from the affected area.
Early diagnosis and treatment can significantly improve outcomes and prevent complications associated with thrombophlebitis.