High platelet count, also known as thrombocythemia, is a condition where the body produces an excessive number of platelets. Platelets are small blood cells that play a crucial role in blood clotting. While having an adequate number of platelets is essential for preventing excessive bleeding, an abnormally high count can lead to complications such as blood clots or bleeding disorders. In this article, we will explore the causes, symptoms, and treatment options for this condition.
Understanding High Platelet Count
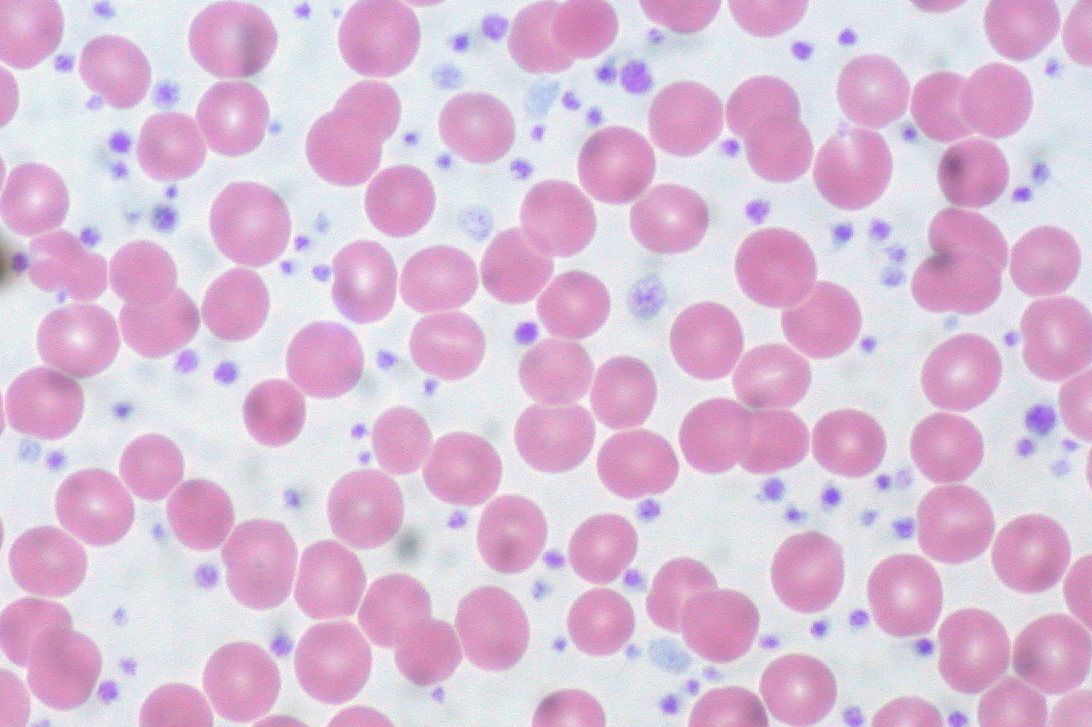
Platelets, also referred to as thrombocytes, are produced in the bone marrow. They circulate in the bloodstream and help stop bleeding by forming clots at sites of injury. A normal platelet count typically ranges between 150,000 and 450,000 platelets per microliter of blood. When the platelet count exceeds this range, it is considered elevated, and when it surpasses 600,000 platelets per microliter, it may be diagnosed as thrombocythemia.
There are two main types of high platelet counts:
- Primary Thrombocythemia: This occurs when the bone marrow produces too many platelets due to a disorder within the bone marrow itself.
- Secondary Thrombocytosis: This happens when an underlying condition, such as infection, inflammation, or another medical issue, stimulates the production of platelets.
Causes of High Platelet Count
The causes of high platelet count vary depending on whether it is primary or secondary. Below are some common factors associated with each type:
Primary Thrombocythemia
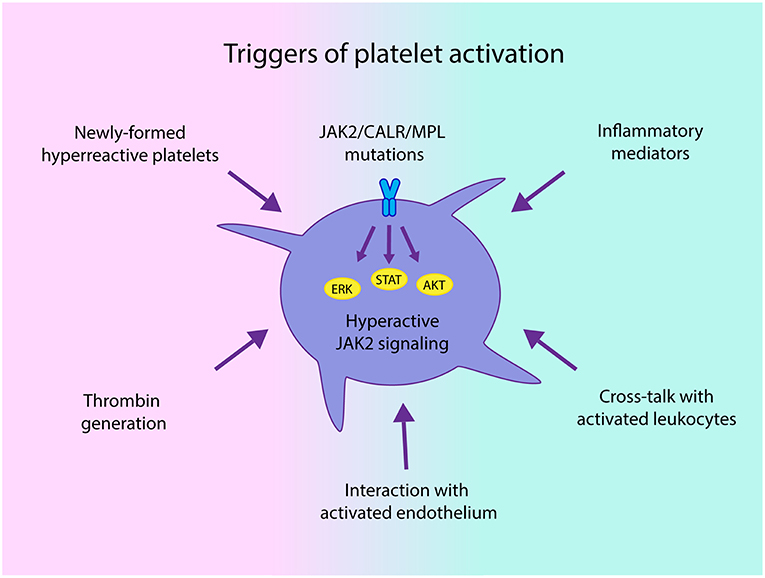
This condition is often linked to genetic mutations that affect the bone marrow’s ability to regulate platelet production. Some key causes include:
- JAK2 Mutation: A mutation in the JAK2 gene is commonly found in individuals with primary thrombocythemia. This mutation leads to uncontrolled growth of megakaryocytes, the cells responsible for producing platelets.
- CALR Mutation: Another genetic mutation, CALR, can also cause abnormal platelet production.
- Essential Thrombocythemia: This is a specific type of primary thrombocythemia characterized by excessive platelet production without an identifiable underlying cause.
Secondary Thrombocytosis
Secondary thrombocytosis is usually a reaction to an external factor rather than a problem originating in the bone marrow. Common triggers include:
- Infections: Bacterial or viral infections can temporarily increase platelet production as part of the body’s immune response.
- Inflammatory Diseases: Conditions like rheumatoid arthritis or inflammatory bowel disease can stimulate platelet production.
- Anemia: Iron deficiency anemia often leads to increased platelet counts as the body attempts to compensate for low red blood cell levels.
- Surgery or Trauma: Recovery from surgery or physical trauma can sometimes result in elevated platelet counts.
- Cancer: Certain cancers, particularly those affecting the bone marrow, can cause secondary thrombocytosis.
Symptoms of High Platelet Count
Many individuals with high platelet counts may not experience any noticeable symptoms, especially if the elevation is mild. However, when symptoms do occur, they can vary widely and may include:
- Blood Clots: Excessive platelets can lead to the formation of blood clots in arteries or veins. These clots can block blood flow and cause serious complications such as heart attacks, strokes, or deep vein thrombosis.
- Bleeding Issues: Paradoxically, despite having too many platelets, some people may experience abnormal bleeding. This can manifest as nosebleeds, gum bleeding, or easy bruising.
- Headaches and Dizziness: Blood clots in smaller vessels can reduce blood flow to the brain, leading to headaches, dizziness, or even transient ischemic attacks.
- Numbness or Tingling: Reduced blood flow to extremities may cause sensations of numbness or tingling in the hands and feet.
- Fatigue: Some individuals report feeling unusually tired or weak, which may be related to underlying conditions contributing to the high platelet count.
Diagnosis of High Platelet Count
To diagnose high platelet count, healthcare providers typically perform a series of tests to determine the underlying cause and assess the severity of the condition. These diagnostic steps may include:
- Blood Tests: A complete blood count is used to measure the number of platelets in the blood. Additional tests may evaluate the size and function of the platelets.
- Bone Marrow Biopsy: In cases of suspected primary thrombocythemia, a sample of bone marrow may be taken to examine the activity of megakaryocytes.
- Genetic Testing: If primary thrombocythemia is suspected, genetic testing may be conducted to identify mutations such as JAK2 or CALR.
- Evaluation of Underlying Conditions: For secondary thrombocytosis, doctors will investigate potential triggers, such as infections, inflammatory diseases, or other medical issues.
Treatment Options for High Platelet Count
Treatment for high platelet count depends on the type, severity, and underlying cause of the condition. The goal is to manage symptoms, prevent complications, and address the root cause if possible.
Managing Primary Thrombocythemia
For individuals with primary thrombocythemia, treatment focuses on reducing the risk of blood clots and managing symptoms. Common approaches include:
- Medications to Lower Platelet Count: Drugs such as hydroxyurea or anagrelide may be prescribed to decrease platelet production.
- Aspirin Therapy: Low-dose aspirin is often recommended to reduce the risk of blood clots by inhibiting platelet aggregation.
- Regular Monitoring: Frequent blood tests and check-ups are necessary to monitor platelet levels and adjust treatment as needed.
Treating Secondary Thrombocytosis
In cases of secondary thrombocytosis, treatment primarily involves addressing the underlying condition causing the elevated platelet count. Examples include:
- Treating Infections: Antibiotics or antiviral medications may be used to resolve infections that are stimulating platelet production.
- Managing Inflammatory Diseases: Anti-inflammatory drugs or immunosuppressive therapies can help control conditions like rheumatoid arthritis or Crohn’s disease.
- Correcting Anemia: Iron supplements or dietary changes may be recommended to treat iron deficiency anemia.
Lifestyle Modifications
In addition to medical treatments, certain lifestyle adjustments can help reduce the risks associated with high platelet counts:
- Healthy Diet: Consuming a balanced diet rich in fruits, vegetables, and whole grains supports overall health and reduces inflammation.
- Regular Exercise: Physical activity improves circulation and lowers the risk of blood clots.
- Avoiding Smoking and Alcohol: Both smoking and excessive alcohol consumption can exacerbate cardiovascular risks associated with high platelet counts.
Potential Complications of High Platelet Count
If left untreated, high platelet count can lead to several complications, including:
- Blood Clots: These can obstruct blood vessels and lead to life-threatening events such as heart attacks, strokes, or pulmonary embolisms.
- Bleeding Disorders: Although less common, some individuals may develop bleeding problems due to dysfunctional platelets.
- Progression to Other Blood Disorders: In rare cases, primary thrombocythemia can evolve into more severe conditions, such as myelofibrosis or acute leukemia.
When to Seek Medical Attention
It is important to consult a healthcare provider if you experience symptoms such as persistent headaches, unexplained fatigue, frequent nosebleeds, or unusual bruising. Early diagnosis and treatment can significantly reduce the risk of complications and improve quality of life.
Final Thoughts
High platelet count is a complex condition that requires careful evaluation and management. By understanding its causes, recognizing its symptoms, and adhering to appropriate treatment plans, individuals can effectively navigate this health challenge. Regular communication with healthcare professionals ensures timely interventions and optimal outcomes.