Spondylosis, often abbreviated as SP, is a term used to describe the degenerative changes that occur in the spine as a natural part of aging. While these changes are common and may not always cause symptoms, they can lead to discomfort, pain, and reduced mobility in some individuals. This article delves into the causes, symptoms, risk factors, and effects of spinal degeneration, offering a comprehensive understanding of this condition.
What is Spondylosis?
Spondylosis refers to the wear and tear of the spinal discs, joints, and bones. It is a broad term that encompasses various types of spinal degeneration, including osteoarthritis of the spine, degenerative disc disease, and bone spurs. These changes typically occur in the cervical (neck), thoracic (mid-back), or lumbar (lower back) regions of the spine.
The spine is made up of vertebrae separated by intervertebral discs, which act as cushions to absorb shock and allow flexibility. Over time, these discs lose water content and elasticity, leading to thinning and increased susceptibility to damage. Additionally, the joints between the vertebrae, known as facet joints, may develop arthritis, and bone spurs may form as the body attempts to stabilize the affected area.
Types of Spondylosis
- Cervical Spondylosis: Affects the neck region and is often associated with stiffness, pain, and nerve compression.
- Thoracic Spondylosis: Involves the mid-back and is less common but can lead to discomfort and restricted movement.
- Lumbar Spondylosis: Occurs in the lower back and is frequently linked to sciatica, where pain radiates down the legs.
Causes of Spinal Degeneration
Several factors contribute to the development of spondylosis. While aging is the primary cause, other elements can accelerate the degenerative process.
Aging
As people grow older, the structures of the spine naturally deteriorate. The intervertebral discs lose hydration and elasticity, making them more prone to tears and bulges. The cartilage in the facet joints also wears down, leading to inflammation and stiffness.
Injury or Trauma
Past injuries to the spine, such as fractures or dislocations, can increase the likelihood of developing spondylosis. Even minor repetitive strain from poor posture or heavy lifting can contribute to spinal degeneration over time.
Genetics
Some individuals are genetically predisposed to spinal issues, making them more susceptible to early-onset spondylosis. Family history can play a significant role in determining who is at higher risk.
Lifestyle Factors
Certain lifestyle choices can exacerbate spinal degeneration. Sedentary behavior, obesity, smoking, and poor ergonomics can all place additional stress on the spine, accelerating wear and tear.
Symptoms of Spondylosis
The symptoms of spondylosis vary depending on the location and severity of the degeneration. Some individuals may experience no symptoms at all, while others may face chronic pain and functional limitations.
Common Symptoms
- Pain: Persistent or intermittent pain in the affected area of the spine.
- Stiffness: Reduced flexibility and difficulty moving the neck or back.
- Numbness or Tingling: Often caused by nerve compression, leading to sensations in the arms, legs, or other areas.
- Muscle Weakness: Weakened muscles due to nerve involvement.
- Headaches: Particularly in cases of cervical spondylosis, headaches may originate from neck tension.
When Symptoms Worsen
In advanced cases, spondylosis can lead to complications such as spinal stenosis (narrowing of the spinal canal), herniated discs, or radiculopathy (pinched nerves). These conditions can significantly impact quality of life, causing severe pain, loss of balance, or even bladder and bowel dysfunction.
Risk Factors for Developing Spondylosis
While aging is inevitable, certain factors can increase the risk of developing spondylosis earlier or experiencing more severe symptoms.
Age
Individuals over the age of forty are more likely to experience signs of spinal degeneration. By the age of sixty, most people show some degree of spondylosis on imaging tests, even if they are asymptomatic.
Occupation
Jobs that involve repetitive motions, heavy lifting, or prolonged sitting can place undue stress on the spine, increasing the likelihood of degeneration.
Obesity
Excess body weight places additional pressure on the spine, accelerating the breakdown of discs and joints.
Smoking
Smoking reduces blood flow to the spinal tissues, impairing their ability to heal and regenerate. This can hasten the degenerative process.
Poor Posture
Slouching or maintaining improper posture for extended periods can strain the spine, contributing to early-onset spondylosis.
Effects of Spondylosis on Daily Life
Spondylosis can have a profound impact on an individual’s daily activities, mental health, and overall well-being. Understanding these effects can help patients and caregivers better manage the condition.
Physical Limitations
One of the most immediate effects of spondylosis is reduced physical function. Simple tasks like bending, lifting, or turning the head may become challenging. Chronic pain can also interfere with sleep, leading to fatigue and decreased productivity.
Emotional and Psychological Impact
Living with persistent pain and limited mobility can take a toll on mental health. Many individuals with spondylosis experience anxiety, depression, or feelings of frustration due to their inability to perform everyday activities.
Impact on Work and Social Life
For those whose jobs require physical labor, spondylosis can make it difficult to continue working. Even desk jobs may become problematic if prolonged sitting exacerbates symptoms. Socially, individuals may withdraw from activities they once enjoyed, leading to isolation and loneliness.
Diagnosis of Spondylosis
Diagnosing spondylosis typically involves a combination of medical history review, physical examination, and imaging tests. Early diagnosis is crucial for effective management and prevention of further complications.
Medical History and Physical Examination
A healthcare provider will begin by asking about symptoms, their duration, and any factors that worsen or alleviate them. During the physical exam, the doctor will assess range of motion, reflexes, muscle strength, and areas of tenderness.
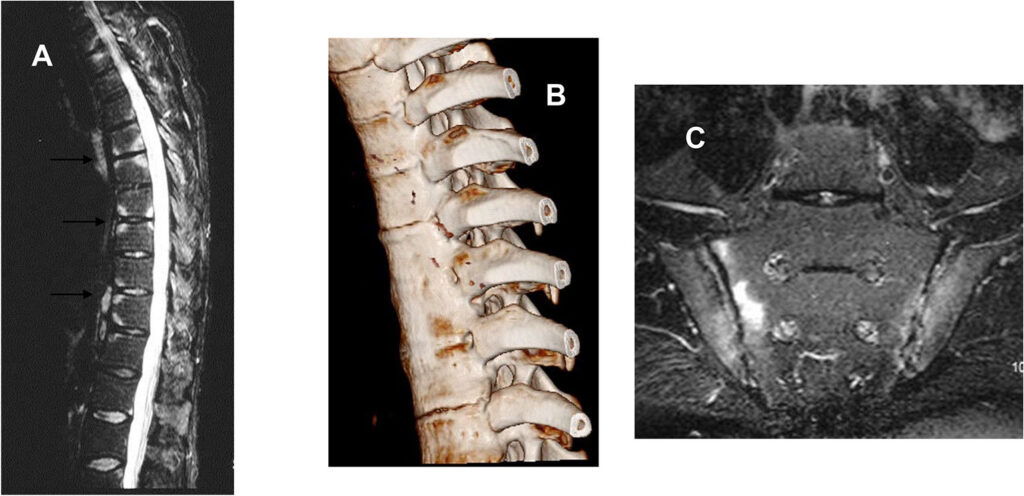
Imaging Tests
Imaging studies are essential for confirming the presence and extent of spinal degeneration. Common tests include:
- X-rays: Used to identify bone spurs, disc space narrowing, and alignment issues.
- Magnetic Resonance Imaging (MRI): Provides detailed images of soft tissues, including discs, nerves, and ligaments.
- Computed Tomography (CT) Scan: Offers cross-sectional views of the spine, useful for detecting bone abnormalities.
Treatment Options for Spondylosis
While there is no cure for spondylosis, various treatments can help manage symptoms and improve quality of life. The choice of treatment depends on the severity of the condition and the patient’s specific needs.
Conservative Treatments
Non-surgical approaches are typically the first line of defense against spondylosis. These include:
- Physical Therapy: Exercises to strengthen core muscles, improve flexibility, and reduce pain.
- Medications: Over-the-counter pain relievers, anti-inflammatory drugs, or prescription medications for severe cases.
- Heat and Cold Therapy: Applying heat or ice packs to alleviate pain and inflammation.
- Ergonomic Adjustments: Modifying workstations or daily habits to reduce strain on the spine.
Interventional Procedures
For individuals who do not respond to conservative treatments, interventional procedures may be recommended:
- Epidural Steroid Injections: Administered to reduce inflammation around compressed nerves.
- Facet Joint Injections: Targeted injections to relieve pain originating from arthritic facet joints.
Surgical Interventions
In severe cases where nerve compression or spinal instability is present, surgery may be necessary. Common surgical options include:
- Discectomy: Removal of a portion of a herniated disc to relieve nerve pressure.
- Spinal Fusion: Joining two or more vertebrae to stabilize the spine.
- Laminectomy: Removal of part of the vertebral bone to create more space for nerves.
Preventing and Managing Spondylosis
While spondylosis cannot be entirely prevented, certain measures can slow its progression and minimize its impact on daily life.
Exercise and Physical Activity
Regular exercise strengthens the muscles supporting the spine, improves flexibility, and promotes overall spinal health. Low-impact activities like swimming, yoga, and walking are particularly beneficial.
Maintaining a Healthy Weight
Weight management reduces stress on the spine, decreasing the risk of accelerated degeneration.
Proper Posture and Ergonomics
Using ergonomic furniture, practicing good posture, and taking frequent breaks during prolonged sitting can protect the spine from unnecessary strain.
Quitting Smoking
Smoking cessation improves blood flow to the spine, aiding in tissue repair and regeneration.
Regular Check-Ups
Frequent visits to a healthcare provider can help monitor spinal health and address any emerging issues promptly.