Rett Syndrome, often abbreviated as RTT, is a rare neurodevelopmental disorder that primarily affects females. It is characterized by a range of physical and cognitive impairments that become evident in early childhood. While the condition is complex and challenging, understanding its symptoms, causes, and available care options can empower families, caregivers, and healthcare professionals to provide better support for those affected. This article delves into the intricacies of this condition, shedding light on its manifestations, underlying causes, and strategies for managing the disorder.
Understanding Rett Syndrome
Rett Syndrome was first described by Austrian pediatrician Andreas Rett in 1966. It is a genetic disorder that impacts brain development, leading to severe impairments in motor skills, communication, and cognitive abilities. The condition typically manifests after a period of seemingly normal early development, making it particularly perplexing for parents and caregivers who may initially believe their child is developing typically.
Key Characteristics of the Disorder
The hallmark of this syndrome is its progressive nature. Children with this condition often experience a regression in skills they had previously acquired. Below are some of the most common characteristics:
- Loss of Hand Skills: One of the earliest signs is the loss of purposeful hand movements. Children may begin wringing their hands or clapping repetitively.
- Communication Challenges: Speech and language development are significantly impaired, and many children lose the ability to speak altogether.
- Motor Difficulties: Problems with coordination and movement, such as difficulty walking or maintaining balance, are common.
- Social Withdrawal: Affected individuals may exhibit reduced eye contact and diminished interest in social interactions.
Symptoms of Rett Syndrome
The symptoms of this condition vary widely in severity and progression. However, they generally follow a predictable pattern, divided into four stages. Understanding these stages can help caregivers and healthcare providers anticipate changes and adapt care strategies accordingly.
Stage 1: Early Onset (6 to 18 Months)
In the initial stage, subtle changes may occur that are often overlooked. These include:
- Delayed achievement of developmental milestones, such as sitting or crawling.
- Reduced interest in toys or surroundings.
- Slowed head growth, which may be an early indicator of the condition.
Stage 2: Rapid Deterioration (1 to 4 Years)
This stage is marked by a noticeable decline in skills. Key symptoms include:
- Loss of previously acquired speech and motor skills.
- Development of repetitive hand movements, such as wringing, clapping, or mouthing hands.
- Increased irritability and crying spells.
- Breathing irregularities, such as holding breath or hyperventilating.
Stage 3: Plateau (2 to 10 Years)
During this phase, the progression of symptoms stabilizes. While challenges persist, some individuals may show slight improvements in behavior and communication. Common features include:
- Improved eye contact and interaction with others.
- Reduced frequency of seizures, if present.
- Continued difficulties with mobility and coordination.
Stage 4: Late Motor Deterioration (After 10 Years)
In the final stage, individuals may experience further declines in motor function but often maintain their cognitive and communication abilities. Symptoms include:
- Increased muscle weakness and rigidity.
- Loss of the ability to walk in some cases.
- Persistent breathing irregularities and scoliosis.
Causes of Rett Syndrome
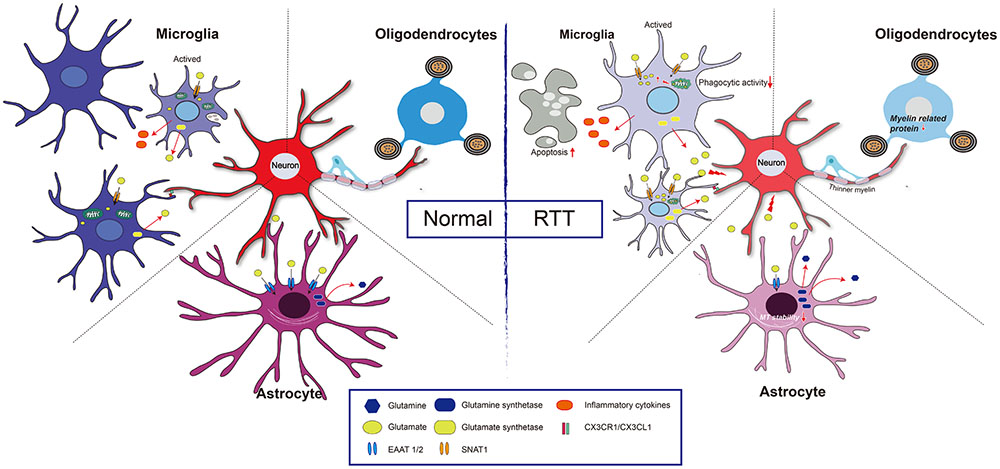
This condition is primarily caused by mutations in a specific gene located on the X chromosome. The gene responsible is known as MECP2, which plays a crucial role in brain development and function. Mutations in this gene disrupt the normal functioning of neurons, leading to the characteristic symptoms of the syndrome.
Genetic Factors
The majority of cases are sporadic, meaning the mutation occurs randomly and is not inherited from the parents. In rare instances, the mutation can be passed down from an unaffected mother who carries the altered gene. Because males have only one X chromosome, mutations in the MECP2 gene are typically fatal for male embryos, which explains why the condition predominantly affects females.
Role of MECP2 Gene
The MECP2 gene provides instructions for producing a protein that regulates the activity of other genes in the brain. This protein is essential for the normal development of nerve cells and the maintenance of synapses, which are the connections between neurons. When the MECP2 gene is mutated, the resulting protein may be absent or dysfunctional, leading to widespread abnormalities in brain function.
Diagnosis of Rett Syndrome
Diagnosing this condition involves a combination of clinical evaluation and genetic testing. Since the symptoms can overlap with other neurological disorders, a thorough assessment is critical for accurate identification.
Clinical Evaluation
Healthcare providers will assess the child’s developmental history, physical symptoms, and behavioral patterns. Key indicators include:
- Regression in motor and communication skills.
- Presence of repetitive hand movements.
- Slowed head growth or microcephaly.
Genetic Testing
Confirming the diagnosis requires genetic testing to identify mutations in the MECP2 gene. This test involves analyzing a sample of the child’s DNA, usually obtained through a blood draw. If a mutation is detected, it confirms the presence of the condition.
Treatment and Care Options
While there is currently no cure for this syndrome, various interventions can help manage symptoms and improve quality of life. A multidisciplinary approach involving medical professionals, therapists, and caregivers is essential for addressing the diverse needs of affected individuals.
Medical Management
Medical care focuses on alleviating specific symptoms and preventing complications. Common interventions include:
- Anticonvulsant Medications: To manage seizures, which are common in individuals with this condition.
- Physical Therapy: To maintain mobility and prevent joint contractures.
- Occupational Therapy: To improve fine motor skills and promote independence in daily activities.
- Speech Therapy: To enhance communication abilities, even if verbal speech is limited.
Nutritional Support
Many individuals with this condition experience feeding difficulties due to problems with chewing, swallowing, or gastrointestinal motility. Nutritional support may involve:
- Modifying the texture of food to make it easier to eat.
- Using feeding tubes in severe cases to ensure adequate nutrition and hydration.
Behavioral and Educational Interventions
Behavioral therapies and specialized education programs can help individuals with this syndrome develop new skills and improve their overall well-being. These interventions often focus on:
- Enhancing social interaction and engagement.
- Providing structured routines to reduce anxiety and improve predictability.
- Using assistive communication devices to facilitate nonverbal communication.
Support for Families and Caregivers
Caring for a child with this condition can be emotionally and physically demanding. Families and caregivers require support to navigate the challenges associated with the disorder. Resources and strategies include:
Support Groups
Connecting with other families who are facing similar challenges can provide emotional support and practical advice. Support groups, both online and in-person, offer a platform for sharing experiences and coping strategies.
Respite Care
Respite care services allow caregivers to take breaks while ensuring their loved ones receive proper attention and care. This can help prevent burnout and improve the overall well-being of caregivers.
Educational Resources
Access to reliable information about the condition, treatment options, and care strategies is crucial for families. Organizations dedicated to raising awareness about this syndrome often provide educational materials and workshops.
Ongoing Research and Future Directions
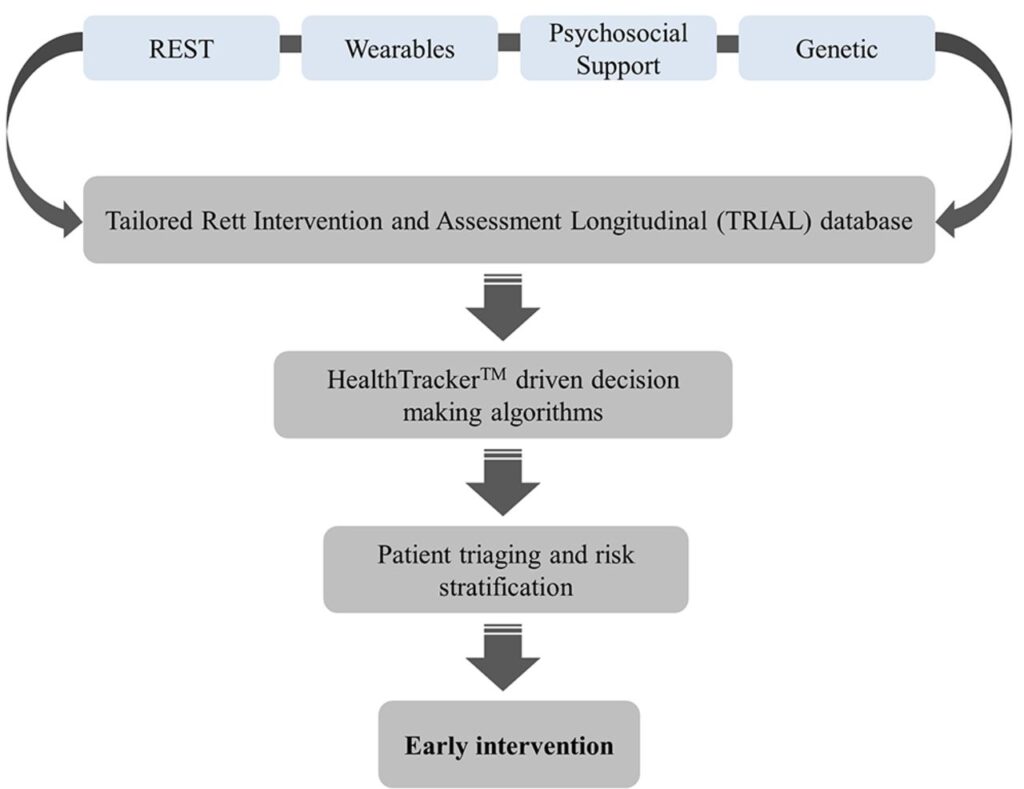
Research into this syndrome is ongoing, with scientists exploring potential treatments and therapies to address the underlying genetic causes. Some promising areas of investigation include:
- Gene therapy approaches aimed at correcting mutations in the MECP2 gene.
- Pharmacological treatments to improve neuronal function and alleviate symptoms.
- Studies on the role of environmental factors in modifying the severity of the condition.
As our understanding of this syndrome continues to evolve, there is hope for more effective interventions and improved outcomes for affected individuals.