Raynaud’s Phenomenon, often abbreviated as RP, is a condition that affects blood flow to certain parts of the body, most commonly the fingers and toes. This disorder causes these areas to feel cold and numb in response to cold temperatures or stress. While it is not life-threatening, Raynaud’s Phenomenon can significantly impact quality of life if left untreated. In this article, we will explore the underlying causes, common symptoms, diagnostic methods, and available treatments for this condition.
Understanding Raynaud’s Phenomenon
Raynaud’s Phenomenon occurs when small blood vessels, particularly those in the extremities, overreact to cold temperatures or emotional stress. This reaction causes the vessels to narrow, reducing blood flow to the affected areas. The reduced circulation leads to discoloration, pain, and discomfort. There are two types of this condition: primary and secondary. Primary Raynaud’s Phenomenon occurs on its own without any underlying medical condition, while secondary Raynaud’s Phenomenon is linked to other health issues, such as autoimmune diseases.
Primary vs. Secondary Raynaud’s Phenomenon
- Primary Raynaud’s Phenomenon: Also known as Raynaud’s disease, this form is more common and tends to be less severe. It typically develops in people under the age of 30 and does not usually lead to serious complications.
- Secondary Raynaud’s Phenomenon: This type is associated with other medical conditions, such as scleroderma, lupus, or rheumatoid arthritis. It tends to appear later in life and may cause more severe symptoms.
Causes of Raynaud’s Phenomenon
The exact cause of Raynaud’s Phenomenon is not fully understood, but several factors contribute to its development. These include environmental triggers, genetic predispositions, and underlying medical conditions.
Environmental Triggers
Cold temperatures and stress are the most common triggers for episodes of Raynaud’s Phenomenon. When exposed to cold, the body naturally tries to conserve heat by constricting blood vessels in the extremities. In individuals with this condition, the response is exaggerated, leading to excessive narrowing of the blood vessels. Similarly, emotional stress can cause the same reaction, even in the absence of cold exposure.
Genetic Factors
Some evidence suggests that genetics may play a role in the development of Raynaud’s Phenomenon. Individuals with a family history of the condition are more likely to experience it themselves. However, the specific genes involved have not been fully identified.
Underlying Medical Conditions
Secondary Raynaud’s Phenomenon is often linked to other health issues. Some of the most common conditions associated with this form include:
- Scleroderma: A connective tissue disorder that causes hardening and tightening of the skin.
- Lupus: An autoimmune disease that causes inflammation and damage to various organs.
- Rheumatoid Arthritis: A chronic inflammatory disorder affecting the joints.
- Atherosclerosis: A condition characterized by the buildup of plaque in the arteries.
Symptoms of Raynaud’s Phenomenon
The symptoms of Raynaud’s Phenomenon are typically triggered by exposure to cold or stress. They vary in severity and duration, depending on the individual and the type of the condition.
Common Symptoms
- Cold Fingers or Toes: The affected areas become noticeably colder than the rest of the body.
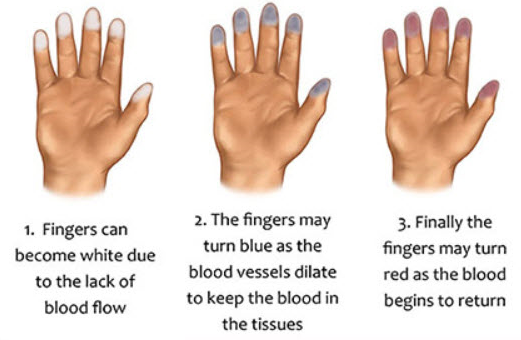
- Color Changes: The skin may turn white, blue, or red during an episode. White indicates reduced blood flow, blue signifies oxygen deprivation, and red occurs when blood flow returns.
- Numbness or Tingling: A lack of sensation or a pins-and-needles feeling often accompanies the color changes.
- Pain or Discomfort: As blood flow returns, the affected areas may throb, ache, or feel swollen.
Less Common Symptoms
In severe cases, prolonged episodes of reduced blood flow can lead to complications such as ulcers or sores on the fingertips or toes. These complications are more common in individuals with secondary Raynaud’s Phenomenon.
Diagnosis of Raynaud’s Phenomenon
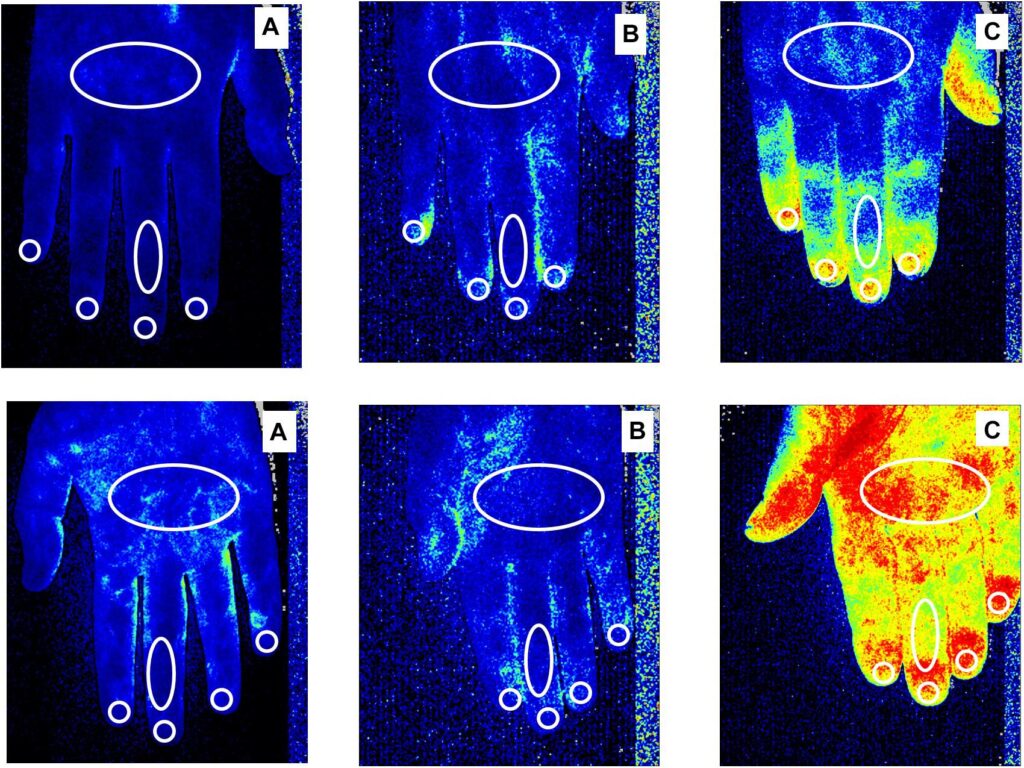
Diagnosing Raynaud’s Phenomenon involves a combination of physical examinations, patient history, and specialized tests. Since the symptoms can mimic those of other conditions, a thorough evaluation is essential for accurate diagnosis.
Physical Examination and Patient History
A healthcare provider will begin by examining the affected areas and asking about the patient’s symptoms, including their frequency, duration, and triggers. They may also inquire about family history and any underlying medical conditions.
Cold Simulation Test
This test involves exposing the hands or feet to cold temperatures to observe the body’s response. If the blood vessels constrict excessively, it may indicate Raynaud’s Phenomenon.
Blood Tests
Blood tests can help identify underlying conditions that may be causing secondary Raynaud’s Phenomenon. For example, tests for antinuclear antibodies (ANA) and erythrocyte sedimentation rate (ESR) can detect autoimmune disorders like lupus or scleroderma.
Capillaroscopy
This non-invasive procedure involves examining the tiny blood vessels at the base of the fingernails using a microscope. Abnormalities in these capillaries can provide clues about the presence of Raynaud’s Phenomenon and its potential connection to other diseases.
Treatments for Raynaud’s Phenomenon
While there is no cure for Raynaud’s Phenomenon, several treatment options can help manage symptoms and reduce the frequency and severity of episodes. The choice of treatment depends on the type and severity of the condition, as well as the presence of underlying health issues.
Lifestyle Modifications
Making simple lifestyle changes can significantly improve symptoms for many individuals. These include:
- Dressing warmly in cold weather, especially protecting the hands and feet.
- Avoiding sudden temperature changes, such as moving from a warm room to a cold environment.
- Using gloves or hand warmers when handling cold objects.
- Practicing stress-reduction techniques, such as yoga or meditation.
Medications
For individuals with severe symptoms, medications may be prescribed to improve blood flow and prevent complications. Commonly used drugs include:
- Calcium channel blockers: These medications relax and widen the blood vessels, improving circulation.
- Vasodilators: Drugs like nitroglycerin can help open up blood vessels in the affected areas.
- Alpha-blockers: These medications counteract the effects of norepinephrine, a hormone that constricts blood vessels.
Treatment of Underlying Conditions
If Raynaud’s Phenomenon is secondary to another medical condition, treating the underlying issue is crucial. For example, managing scleroderma or lupus with appropriate medications can help alleviate symptoms of Raynaud’s Phenomenon.
Surgical Options
In rare cases where symptoms are severe and unresponsive to other treatments, surgical procedures may be considered. One option is sympathectomy, which involves cutting the nerves responsible for constricting blood vessels in the affected areas. Another option is nerve-blocking injections, which temporarily block the nerves causing the blood vessel constriction.
Preventing Episodes of Raynaud’s Phenomenon
Prevention plays a key role in managing Raynaud’s Phenomenon. By avoiding triggers and adopting healthy habits, individuals can reduce the frequency and severity of episodes.
Protecting Against Cold
Wearing insulated gloves, socks, and hats can help maintain body heat in cold environments. Using heated car seat covers or electric blankets may also be beneficial.
Managing Stress
Stress management techniques, such as deep breathing exercises, mindfulness, and regular physical activity, can help reduce the likelihood of stress-induced episodes.
Healthy Lifestyle Choices
Quitting smoking, maintaining a balanced diet, and exercising regularly can improve overall circulation and reduce the risk of complications.