Rapid Eye Movement Sleep Behavior Disorder, commonly abbreviated as RBD, is a fascinating yet potentially serious sleep disorder that affects the way people experience one of the most critical stages of sleep. During this stage, individuals with this condition physically act out vivid dreams, often resulting in disruptive or even dangerous behaviors. While it may sound unusual, understanding the intricacies of this disorder can help individuals and their loved ones navigate its challenges effectively. In this article, we will explore the underlying causes, common symptoms, and available treatments for this condition.
What Happens During REM Sleep?
To fully grasp what makes this disorder unique, it’s essential to understand the role of rapid eye movement sleep. This stage of sleep is characterized by heightened brain activity, vivid dreaming, and temporary muscle paralysis. Normally, during this phase, the body enters a state of atonia, where most muscles are temporarily immobilized. This natural mechanism prevents people from physically acting out their dreams. However, in individuals with this condition, this protective paralysis is either incomplete or entirely absent, leading to physical movements during sleep.
The Science Behind the Disorder
Researchers believe that this disorder occurs due to dysfunction in specific areas of the brainstem, which regulate sleep and muscle control. The brainstem plays a crucial role in maintaining the balance between wakefulness and sleep. When this balance is disrupted, it can lead to abnormal behaviors during sleep. Studies have also linked this condition to neurodegenerative diseases, such as Parkinson’s disease and multiple system atrophy, suggesting a potential connection between this sleep disorder and broader neurological health.
Common Causes of the Disorder
While the exact cause of this condition remains unclear, several factors have been identified as potential contributors. These include:
- Neurological Disorders: Many individuals diagnosed with this condition also exhibit signs of neurodegenerative diseases. This overlap has led researchers to investigate whether this sleep disorder could be an early indicator of conditions like Parkinson’s disease or dementia with Lewy bodies.
- Medications: Certain medications, particularly antidepressants, have been associated with triggering symptoms of this disorder. It’s important for individuals taking these medications to discuss any sleep-related changes with their healthcare provider.
- Genetic Factors: Some evidence suggests that genetics may play a role in predisposing individuals to this condition. Family history can sometimes provide clues about susceptibility.
- Brain Injuries: Trauma to the brain, such as from a stroke or head injury, can disrupt normal sleep patterns and contribute to the development of this disorder.
Environmental and Lifestyle Influences
In addition to biological factors, environmental and lifestyle influences can exacerbate symptoms. Stress, alcohol consumption, and irregular sleep schedules may worsen the severity of this condition. Addressing these external factors can sometimes help reduce the frequency and intensity of episodes.
Symptoms to Watch For
Recognizing the symptoms of this disorder is crucial for early diagnosis and intervention. Common signs include:
- Vivid Dreaming: Individuals often report experiencing highly detailed and intense dreams, which they later act out during sleep.
- Physical Movements: These can range from minor gestures, such as talking or twitching, to more dramatic actions like punching, kicking, or jumping out of bed.
- Nocturnal Injuries: Due to the physical nature of their actions, individuals may accidentally harm themselves or their bed partners.
- Daytime Fatigue: Disrupted sleep patterns can lead to excessive daytime sleepiness and fatigue.
Distinguishing From Other Sleep Disorders
It’s important to differentiate this condition from other sleep disorders, such as night terrors or sleepwalking. Unlike those conditions, which typically occur during non-REM sleep, this disorder specifically arises during the rapid eye movement phase. Additionally, individuals with this condition often recall their dreams in vivid detail, whereas those with night terrors or sleepwalking usually have no memory of their episodes.
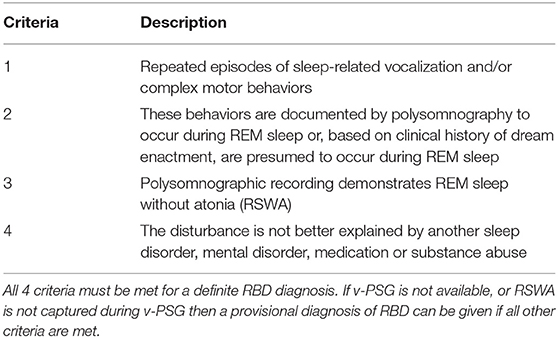
Diagnosing the Condition
Diagnosing this disorder requires a comprehensive evaluation by a healthcare professional. The process typically involves:
- Clinical Interviews: A detailed discussion of symptoms, medical history, and sleep patterns helps doctors identify potential red flags.
- Sleep Studies: Polysomnography, a type of overnight sleep study, is often used to monitor brain activity, muscle movements, and other physiological parameters during sleep. This test can confirm the absence of muscle paralysis during rapid eye movement sleep.
- Partner Observations: Bed partners or family members can provide valuable insights into nighttime behaviors that the individual may not remember.
Challenges in Diagnosis
One of the challenges in diagnosing this condition is that individuals may not always recognize their own symptoms. They might attribute injuries or disturbances to other causes, delaying proper evaluation. Encouraging open communication with healthcare providers is essential for accurate diagnosis and treatment.
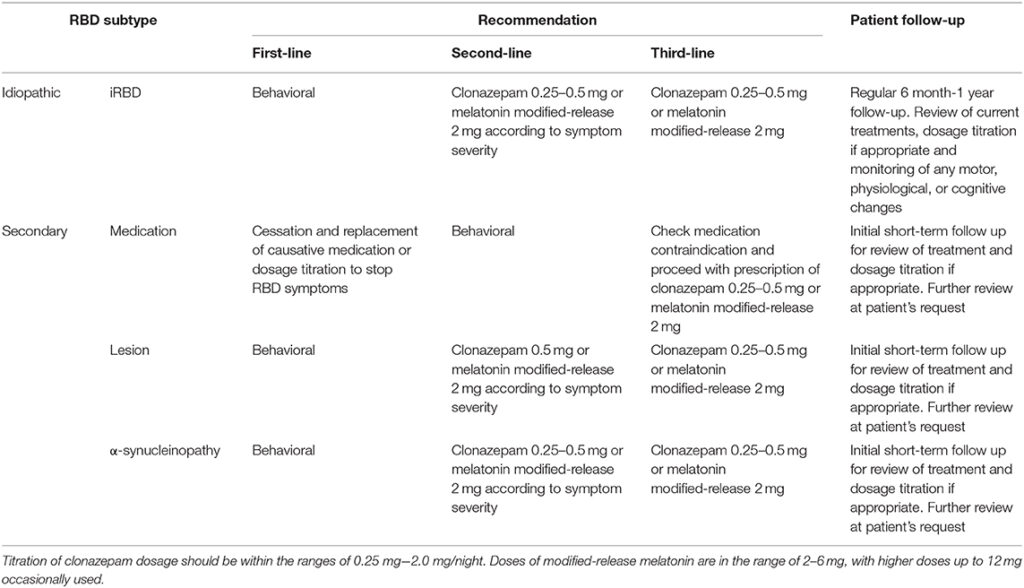
Treatment Options
While there is no cure for this condition, several treatment strategies can help manage symptoms and improve quality of life. These include:
Medications
Doctors often prescribe medications to reduce the frequency and severity of episodes. Common options include:
- Melatonin: This naturally occurring hormone can help regulate sleep cycles and reduce dream enactment behaviors.
- Clonazepam: A benzodiazepine medication, clonazepam is frequently prescribed to suppress muscle activity during sleep. However, it may not be suitable for everyone, especially those with a history of substance abuse.
Lifestyle Modifications
In addition to medications, making certain lifestyle changes can significantly impact symptom management:
- Sleep Environment Adjustments: Removing sharp objects, padding furniture, and ensuring a safe sleeping space can prevent injuries during episodes.
- Stress Reduction: Techniques such as meditation, yoga, or therapy can help lower stress levels, which may reduce symptom severity.
- Regular Sleep Schedule: Maintaining consistent sleep and wake times promotes healthier sleep patterns and minimizes disruptions.
Addressing Underlying Conditions
If this condition is linked to another medical issue, such as a neurological disorder, treating the underlying condition may alleviate symptoms. Regular follow-ups with healthcare providers are essential to monitor progress and adjust treatment plans as needed.
Living With the Disorder
Managing this condition requires patience and collaboration between individuals, their families, and healthcare professionals. Education about the disorder is key to fostering understanding and reducing stigma. Support groups and online communities can also provide valuable resources and emotional support for those navigating this challenging condition.
Tips for Caregivers and Partners
For caregivers and bed partners, living with someone who has this condition can be both physically and emotionally demanding. Here are some tips to help cope:
- Create a Safe Space: Modify the bedroom environment to minimize risks during episodes.
- Communicate Openly: Discuss concerns and observations with the affected individual and their healthcare team.
- Seek Support: Joining support groups or seeking counseling can help caregivers manage stress and maintain their well-being.
Future Directions in Research
Ongoing research into this condition continues to shed light on its causes, progression, and potential treatments. Scientists are exploring the link between this disorder and neurodegenerative diseases, hoping to identify biomarkers that could predict the onset of these conditions. Advances in technology, such as wearable devices that monitor sleep patterns, may also enhance diagnostic accuracy and treatment outcomes.
Promising Therapies
New therapies, including targeted medications and non-pharmacological interventions, are being developed to address the unique challenges of this condition. Clinical trials are underway to test the efficacy of novel treatments, offering hope for improved symptom management in the future.