Pulmonary hypertension, often abbreviated as PH, is a complex and progressive condition that affects the arteries of the lungs and the right side of the heart. This disorder involves elevated blood pressure in the pulmonary arteries, which are responsible for carrying blood from the heart to the lungs. Over time, this increased pressure can lead to significant strain on the heart and may result in severe complications if left untreated. Understanding pulmonary hypertension requires an exploration of its causes, symptoms, and available treatments. In this article, we will delve into each of these aspects to provide a comprehensive overview of this challenging medical condition.

What Is Pulmonary Hypertension?
Pulmonary hypertension occurs when the small arteries in the lungs become narrowed, blocked, or destroyed. This makes it harder for blood to flow through the lungs, increasing the pressure within the pulmonary arteries. As a result, the right ventricle of the heart, which pumps blood to the lungs, must work harder to overcome this resistance. Over time, this extra workload can weaken the heart muscle, leading to heart failure.
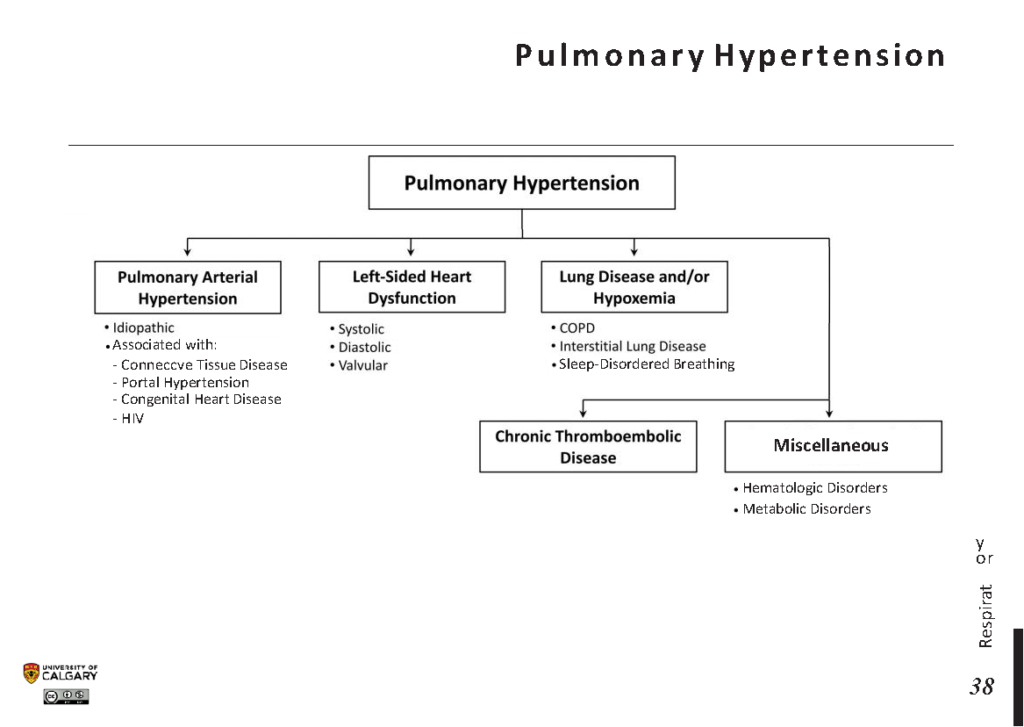
There are several types of pulmonary hypertension, classified based on their underlying causes. These classifications help doctors determine the most appropriate treatment plan for each patient. The World Health Organization has categorized pulmonary hypertension into five groups, each with distinct characteristics and associated conditions.
Types of Pulmonary Hypertension
- Group 1: Pulmonary arterial hypertension, which includes idiopathic cases and those associated with other conditions such as connective tissue diseases or congenital heart defects.
- Group 2: Pulmonary hypertension caused by left-sided heart disease, such as heart failure or valvular disorders.
- Group 3: Pulmonary hypertension related to lung diseases or chronic hypoxia, including chronic obstructive pulmonary disease and interstitial lung disease.
- Group 4: Pulmonary hypertension caused by chronic blood clots in the lungs, also known as chronic thromboembolic pulmonary hypertension.
- Group 5: Pulmonary hypertension associated with various systemic or metabolic disorders, such as sarcoidosis or sickle cell disease.
Causes of Pulmonary Hypertension
The exact cause of pulmonary hypertension can vary depending on the type and group it falls under. In some cases, the condition arises without any identifiable cause, referred to as idiopathic pulmonary arterial hypertension. However, there are numerous factors and underlying conditions that can contribute to the development of pulmonary hypertension.
Genetic Factors
Some individuals may inherit a predisposition to pulmonary arterial hypertension due to genetic mutations. Mutations in specific genes, such as BMPR2, have been linked to familial cases of the condition. If a close family member has been diagnosed with pulmonary arterial hypertension, it is important to discuss this with a healthcare provider, as genetic testing may be recommended.
Underlying Medical Conditions
Several medical conditions can increase the risk of developing pulmonary hypertension. These include:
- Connective tissue diseases, such as scleroderma or lupus
- Congenital heart defects
- Liver disease, particularly cirrhosis
- HIV infection
- Sickle cell disease
- Chronic lung diseases, such as emphysema or pulmonary fibrosis
Lifestyle and Environmental Factors
Certain lifestyle choices and environmental exposures can also contribute to the development of pulmonary hypertension. For example:
- Use of certain appetite suppressants, such as fenfluramine or dexfenfluramine
- Exposure to toxins, such as asbestos or certain chemicals
- Living at high altitudes, which can lead to chronic hypoxia
Symptoms of Pulmonary Hypertension
The symptoms of pulmonary hypertension often develop gradually and may not be noticeable in the early stages of the condition. As the disease progresses, however, symptoms become more pronounced and can significantly impact a person’s quality of life. Recognizing these symptoms early is crucial for timely diagnosis and treatment.
Common Symptoms
- Shortness of breath, especially during physical activity or exertion
- Fatigue and weakness
- Dizziness or fainting spells
- Chest pain or pressure
- Rapid heartbeat or palpitations
- Swelling in the ankles, legs, or abdomen
- Bluish discoloration of the lips or skin, known as cyanosis
When to Seek Medical Attention
If you experience persistent shortness of breath, fatigue, or chest pain, it is important to consult a healthcare provider. These symptoms can be indicative of pulmonary hypertension or other serious conditions. Early diagnosis and treatment can help prevent complications and improve outcomes.
Treatments for Pulmonary Hypertension
While there is no cure for pulmonary hypertension, several treatment options are available to manage symptoms, slow disease progression, and improve quality of life. The choice of treatment depends on the type and severity of the condition, as well as the patient’s overall health.
Medications
Medications play a central role in the management of pulmonary hypertension. These drugs aim to reduce the pressure in the pulmonary arteries, improve blood flow, and alleviate symptoms. Commonly prescribed medications include:
- Vasodilators, which help relax and widen the blood vessels in the lungs
- Endothelin receptor antagonists, which block the effects of endothelin, a substance that narrows blood vessels
- Phosphodiesterase inhibitors, which enhance the effects of nitric oxide to relax blood vessels
- Prostacyclin analogs, which mimic the effects of prostacyclin, a natural substance that dilates blood vessels
- Anticoagulants, which prevent blood clots from forming
Oxygen Therapy
For patients with low oxygen levels in their blood, supplemental oxygen therapy may be recommended. This treatment helps improve oxygenation and reduce strain on the heart.
Lifestyle Modifications
Making certain lifestyle changes can also help manage pulmonary hypertension. These include:
- Avoiding smoking and exposure to secondhand smoke
- Maintaining a healthy weight through diet and exercise
- Limiting salt intake to reduce fluid retention
- Avoiding activities that exacerbate symptoms, such as heavy lifting or extreme temperatures
Surgical Interventions
In severe cases of pulmonary hypertension, surgical interventions may be necessary. These procedures include:
- Atrial septostomy, which creates an opening between the upper chambers of the heart to relieve pressure
- Lung transplantation, which may be considered for patients with advanced disease who do not respond to other treatments
- Pulmonary thromboendarterectomy, a surgery to remove blood clots from the pulmonary arteries in cases of chronic thromboembolic pulmonary hypertension
Regular Monitoring and Follow-Up
Patients with pulmonary hypertension require regular monitoring to assess the effectiveness of treatment and make necessary adjustments. This often involves frequent visits to a specialist, as well as diagnostic tests such as echocardiograms, pulmonary function tests, and blood work.
Living with Pulmonary Hypertension
Living with pulmonary hypertension can be challenging, but with proper management, many individuals are able to lead fulfilling lives. It is important for patients to work closely with their healthcare team to develop a personalized treatment plan. Additionally, joining support groups or connecting with others who have the condition can provide emotional support and valuable insights.
Education about the condition is also key. Understanding the triggers, symptoms, and treatment options empowers patients to take an active role in their care. By staying informed and proactive, individuals with pulmonary hypertension can better navigate the complexities of this condition and maintain their overall well-being.