Psoriatic arthritis, often abbreviated as PsA, is a chronic autoimmune condition that affects individuals who have psoriasis, a skin disorder characterized by red, scaly patches. This type of arthritis causes inflammation in the joints and can lead to pain, stiffness, and swelling. While it shares some similarities with rheumatoid arthritis, psoriatic arthritis has unique features that set it apart. In this article, we will explore the causes, symptoms, diagnosis methods, and treatment options available for managing this condition.
Understanding Psoriatic Arthritis
Psoriatic arthritis is a form of arthritis that occurs in people who already have psoriasis. It typically develops between the ages of thirty and fifty, but it can affect individuals at any age. The exact cause of psoriatic arthritis remains unknown, but researchers believe it is linked to a combination of genetic, immune system, and environmental factors. Understanding these elements is essential to grasp how this condition develops and progresses.
Causes of Psoriatic Arthritis
The development of psoriatic arthritis is influenced by several factors:
- Genetic predisposition: People with a family history of psoriasis or psoriatic arthritis are more likely to develop the condition. Specific genes, such as HLA-B27, have been associated with an increased risk.
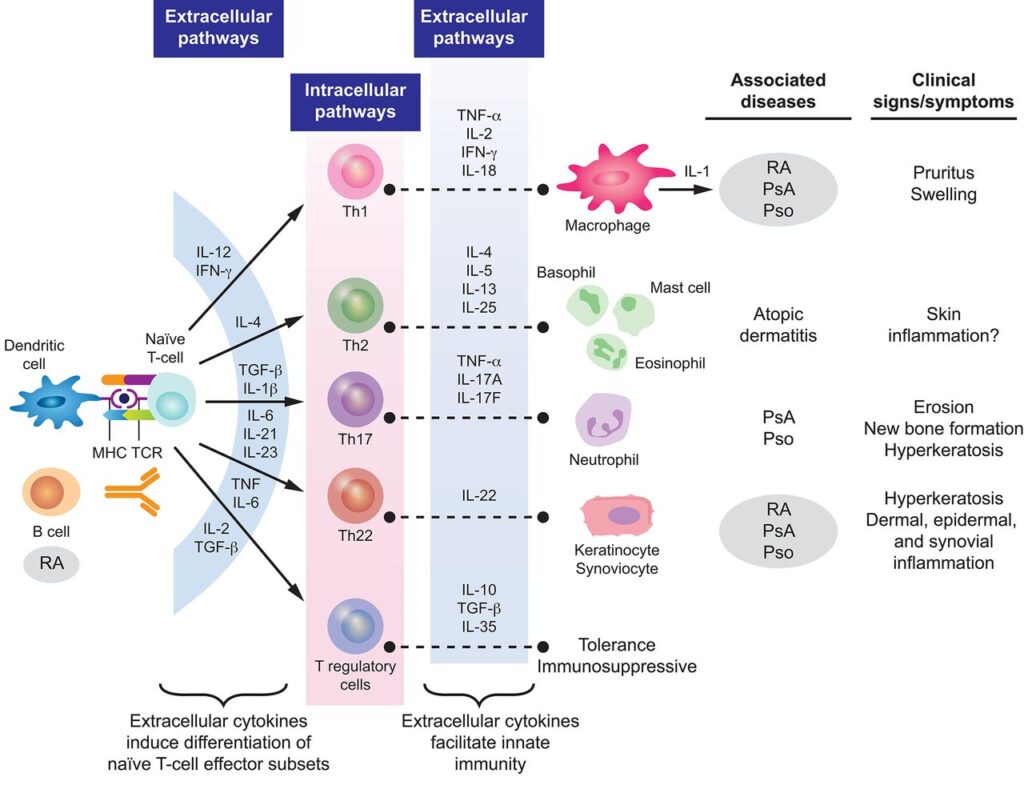
- Immune system dysfunction: Psoriatic arthritis occurs when the immune system mistakenly attacks healthy tissues, particularly the joints and skin. This abnormal immune response leads to inflammation and damage.
- Environmental triggers: Certain infections, injuries, or stressors may trigger the onset of psoriatic arthritis in genetically susceptible individuals. For example, streptococcal infections have been linked to the development of psoriasis and, subsequently, psoriatic arthritis.
Symptoms of Psoriatic Arthritis
The symptoms of psoriatic arthritis can vary widely from person to person. Some individuals experience mild discomfort, while others face severe joint damage and disability. Common signs and symptoms include:
- Joint pain and swelling: Pain and swelling often occur in the fingers, toes, knees, ankles, and lower back. The joints may feel warm to the touch and appear swollen.
- Morning stiffness: Many people with psoriatic arthritis experience stiffness in their joints, especially in the morning or after periods of inactivity.
- Fatigue: Persistent tiredness is a common symptom and can significantly impact daily life.
- Nail changes: Changes in the fingernails and toenails, such as pitting, discoloration, or separation from the nail bed, are frequently observed.
- Tendon and ligament pain: Inflammation of tendons and ligaments, known as enthesitis, can cause pain in areas like the heels, elbows, and knees.
- Reduced range of motion: Over time, joint inflammation can lead to stiffness and a decreased ability to move affected joints freely.
Different Patterns of Joint Involvement
Psoriatic arthritis can manifest in various patterns, affecting different parts of the body:
- Asymmetric arthritis: This pattern involves different joints on each side of the body and is often milder than other forms.
- Symmetric arthritis: Similar to rheumatoid arthritis, this type affects the same joints on both sides of the body.
- Spondylitis: Inflammation of the spine can lead to stiffness and pain in the neck, lower back, and sacroiliac joints.
- Distal interphalangeal predominant: This form primarily affects the joints closest to the nails in the fingers and toes.
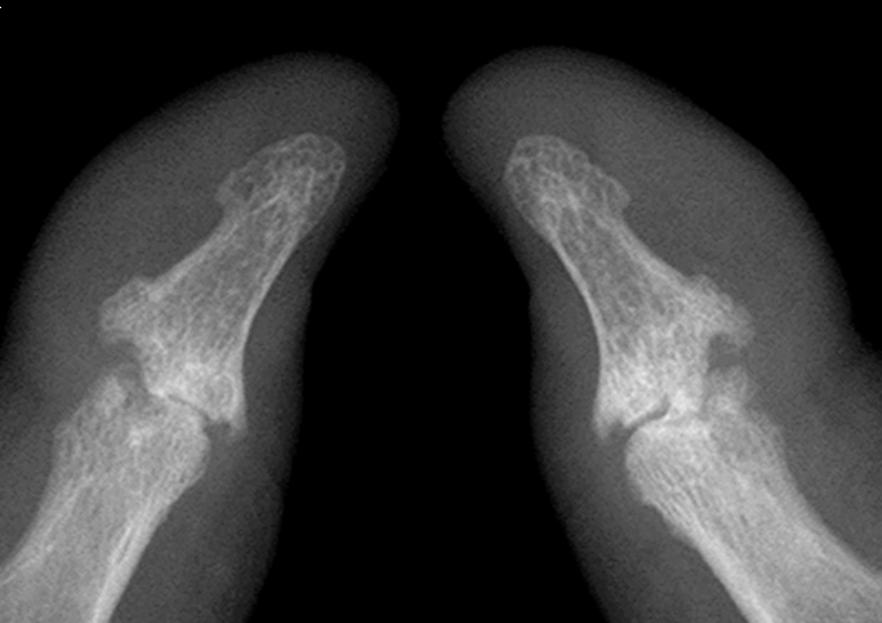
- Arthritis mutilans: A rare and severe form that causes bone loss and deformity in the hands and feet.
Diagnosing Psoriatic Arthritis
Diagnosing psoriatic arthritis can be challenging because its symptoms overlap with those of other types of arthritis. There is no single test to confirm the presence of this condition. Instead, healthcare providers rely on a combination of medical history, physical examinations, imaging tests, and laboratory results to make an accurate diagnosis.
Medical History and Physical Examination
A thorough evaluation begins with a detailed medical history. The doctor will ask about symptoms, their duration, and any family history of psoriasis or arthritis. During the physical examination, they will check for signs of joint swelling, tenderness, and skin changes associated with psoriasis.
Imaging Tests
Imaging tests play a crucial role in diagnosing psoriatic arthritis. These tests help identify joint damage, inflammation, and other abnormalities:
- X-rays: X-rays can reveal bone changes, such as erosions or new bone formation, which are characteristic of psoriatic arthritis.
- Magnetic resonance imaging (MRI): MRI scans provide detailed images of soft tissues, including tendons, ligaments, and cartilage, helping detect early signs of inflammation.
- Ultrasound: Ultrasound imaging can identify joint inflammation and structural damage not visible on X-rays.
Laboratory Tests
While there is no specific blood test for psoriatic arthritis, certain laboratory tests can help rule out other conditions and support the diagnosis:
- Rheumatoid factor (RF) and anti-cyclic citrullinated peptide (anti-CCP): These tests are negative in most cases of psoriatic arthritis but positive in rheumatoid arthritis.
- Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP): Elevated levels of these markers indicate inflammation in the body.
- Joint fluid analysis: Analyzing fluid from an affected joint can help differentiate psoriatic arthritis from gout or infection.
Treatment Options for Psoriatic Arthritis
While there is no cure for psoriatic arthritis, various treatments can help manage symptoms, slow disease progression, and improve quality of life. Treatment plans are tailored to the individual’s needs and may involve medications, lifestyle modifications, and surgical interventions.
Medications
Several types of medications are used to treat psoriatic arthritis:
- Nonsteroidal anti-inflammatory drugs (NSAIDs): These over-the-counter or prescription medications reduce pain and inflammation. Examples include ibuprofen and naproxen.
- Disease-modifying antirheumatic drugs (DMARDs): DMARDs, such as methotrexate, slow the progression of the disease and prevent joint damage.
- Biologic agents: Biologics target specific components of the immune system involved in inflammation. Examples include tumor necrosis factor inhibitors, interleukin inhibitors, and Janus kinase inhibitors.
- Steroids: Corticosteroid injections into affected joints can provide rapid relief from inflammation and pain.
Lifestyle Modifications
In addition to medications, making certain lifestyle changes can help manage psoriatic arthritis:
- Exercise: Regular physical activity helps maintain joint flexibility, strengthen muscles, and reduce stiffness. Low-impact exercises like swimming and yoga are particularly beneficial.
- Weight management: Maintaining a healthy weight reduces stress on the joints and minimizes inflammation.
- Dietary adjustments: Consuming an anti-inflammatory diet rich in fruits, vegetables, whole grains, and omega-3 fatty acids may help alleviate symptoms.
- Stress reduction: Techniques such as meditation, deep breathing, and mindfulness can lower stress levels, which may reduce flare-ups.
Surgical Interventions
In severe cases where joint damage is extensive, surgery may be necessary. Surgical options include:
- Joint replacement: Damaged joints, such as hips or knees, can be replaced with artificial implants to restore function.
- Tendon repair: Surgery may be required to repair or reconstruct damaged tendons and ligaments.
Emerging Therapies
Research into psoriatic arthritis is ongoing, and new therapies are continually being developed. These include novel biologic agents, small-molecule drugs, and personalized medicine approaches aimed at targeting specific pathways involved in the disease process.
Living with Psoriatic Arthritis
Managing psoriatic arthritis requires a comprehensive approach that addresses both physical and emotional well-being. Support groups, counseling, and education about the condition can empower individuals to take control of their health and live fulfilling lives despite the challenges posed by this chronic illness.