Postpartum thyroiditis, often abbreviated as PPT, is a condition that affects some women after giving birth. It involves inflammation of the thyroid gland, leading to temporary changes in its function. This condition can disrupt the delicate hormonal balance in a woman’s body during the postpartum period. Understanding the causes, recognizing the symptoms, getting an accurate diagnosis, and exploring treatment options are essential for managing this condition effectively.
What Is Postpartum Thyroiditis?
Postpartum thyroiditis is a type of thyroid inflammation that occurs within the first year after childbirth. The thyroid gland, located at the base of the neck, plays a critical role in regulating metabolism by producing hormones. In postpartum thyroiditis, the immune system mistakenly attacks the thyroid gland, causing it to become inflamed. This leads to either overproduction or underproduction of thyroid hormones, which can result in a range of physical and emotional symptoms.
How Common Is Postpartum Thyroiditis?
- It affects approximately 5 to 10 percent of women after childbirth.
- Women with a history of autoimmune diseases, such as type 1 diabetes or Hashimoto’s thyroiditis, are at a higher risk.
- Those with a family history of thyroid disorders may also be more susceptible.
Causes of Postpartum Thyroiditis
The exact cause of postpartum thyroiditis is not fully understood, but researchers believe it is related to changes in the immune system during and after pregnancy. Here are some key factors that contribute to its development:
Immune System Changes During Pregnancy
Pregnancy involves significant changes in the immune system to ensure that the mother’s body does not reject the developing fetus. During pregnancy, the immune system becomes less active to tolerate the presence of the baby. After childbirth, the immune system begins to return to its normal state, and this rebound effect can sometimes lead to an autoimmune response. In postpartum thyroiditis, the immune system mistakenly targets the thyroid gland, causing inflammation.
Genetic Predisposition
Some women may have a genetic predisposition to autoimmune conditions. If a woman has a family history of thyroid disorders or other autoimmune diseases, she may be more likely to develop postpartum thyroiditis. Genetic factors can influence how the immune system responds to changes during and after pregnancy.
Hormonal Fluctuations
The dramatic hormonal shifts that occur during pregnancy and after childbirth can also play a role in the development of postpartum thyroiditis. These fluctuations can affect the thyroid gland’s function and make it more vulnerable to inflammation.
Symptoms of Postpartum Thyroiditis
The symptoms of postpartum thyroiditis can vary depending on whether the thyroid is overactive or underactive. The condition typically progresses through two phases: hyperthyroidism (overactive thyroid) followed by hypothyroidism (underactive thyroid). Some women may experience only one phase, while others go through both.
Hyperthyroid Phase
The hyperthyroid phase usually occurs within the first few months after childbirth. During this phase, the inflamed thyroid gland releases excess thyroid hormones into the bloodstream. Symptoms may include:
- Rapid heartbeat or palpitations
- Unexplained weight loss
- Nervousness or irritability
- Tremors or shaking hands
- Increase in sweating or heat intolerance
- Fatigue or weakness
Hypothyroid Phase
The hypothyroid phase typically occurs several months after the hyperthyroid phase. In this phase, the thyroid gland becomes underactive due to damage caused by inflammation. Symptoms may include:
- Fatigue and sluggishness
- Weight gain
- Depression or mood swings
- Dry skin and hair
- Cold intolerance
- Constipation
- Difficulty concentrating or memory problems
Transition Between Phases
Some women may experience a brief period of normal thyroid function between the hyperthyroid and hypothyroid phases. However, others may transition directly from one phase to the other without any noticeable break.
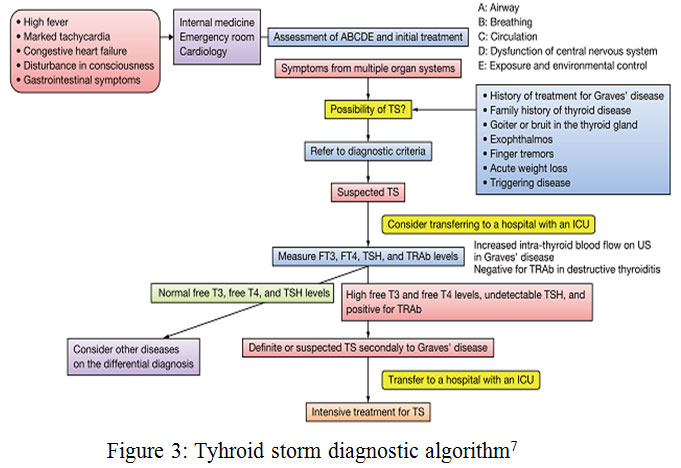
Diagnosis of Postpartum Thyroiditis
Diagnosing postpartum thyroiditis can be challenging because its symptoms often overlap with those of other conditions, such as postpartum depression or fatigue. A thorough evaluation by a healthcare provider is essential for an accurate diagnosis.
Medical History and Physical Examination
The first step in diagnosing postpartum thyroiditis is taking a detailed medical history. The healthcare provider will ask about symptoms, family history of thyroid disorders, and any previous thyroid issues. A physical examination may reveal signs such as an enlarged thyroid gland or changes in heart rate.
Blood Tests
Blood tests are the primary tool for diagnosing postpartum thyroiditis. These tests measure levels of thyroid hormones and antibodies in the blood. Key tests include:
- Thyroid-Stimulating Hormone (TSH): Measures the level of TSH produced by the pituitary gland. Low TSH levels indicate hyperthyroidism, while high levels suggest hypothyroidism.
- Free Thyroxine (T4): Assesses the amount of active thyroid hormone in the blood. High levels indicate hyperthyroidism, while low levels suggest hypothyroidism.
- Thyroid Peroxidase Antibodies (TPO): Detects the presence of antibodies that attack the thyroid gland, which are often elevated in autoimmune thyroid conditions.
Monitoring Over Time
Since postpartum thyroiditis can progress through different phases, repeated blood tests may be necessary to monitor changes in thyroid function over time. This helps healthcare providers determine the appropriate treatment plan.
Treatment Options for Postpartum Thyroiditis
The treatment for postpartum thyroiditis depends on the phase of the condition and the severity of symptoms. In many cases, the condition resolves on its own, but treatment may be necessary to manage symptoms during the hyperthyroid and hypothyroid phases.
Treating the Hyperthyroid Phase
During the hyperthyroid phase, treatment focuses on alleviating symptoms rather than addressing the underlying cause, as the condition is usually temporary. Options include:
- Beta-Blockers: Medications such as propranolol can help reduce symptoms like rapid heartbeat, tremors, and anxiety.
- Monitoring: Regular follow-up appointments are important to ensure that symptoms improve as the thyroid function returns to normal.
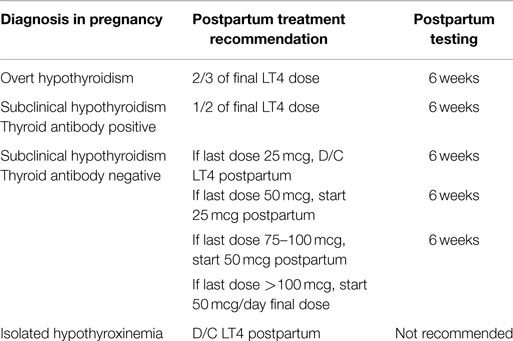
Treating the Hypothyroid Phase
In the hypothyroid phase, treatment may involve thyroid hormone replacement therapy to restore normal hormone levels. Options include:
- Levothyroxine: A synthetic form of thyroid hormone that can help alleviate symptoms of hypothyroidism. The dosage is adjusted based on blood test results.
- Regular Monitoring: Blood tests are used to monitor thyroid hormone levels and adjust medication as needed.
Lifestyle Modifications
In addition to medical treatment, certain lifestyle changes can help manage symptoms of postpartum thyroiditis:
- Balanced Diet: Eating a nutrient-rich diet can support overall health and thyroid function.
- Adequate Rest: Prioritizing sleep and rest is crucial for recovery, especially for new mothers.
- Stress Management: Techniques such as yoga, meditation, or deep breathing exercises can help reduce stress and improve well-being.
Long-Term Outlook
For most women, postpartum thyroiditis resolves within a year. However, some women may develop permanent hypothyroidism and require ongoing treatment with thyroid hormone replacement therapy. Regular follow-up with a healthcare provider is essential to monitor thyroid function and adjust treatment as needed.