Postpartum depression, often abbreviated as PPD, is a serious mental health condition that affects many new mothers after childbirth. It goes beyond the typical “baby blues” and can have profound effects on both the mother and her family. Understanding this condition is crucial for early identification and effective management. In this article, we will explore the causes, symptoms, and care options available for postpartum depression.
Understanding Postpartum Depression
Postpartum depression is a mood disorder that occurs after childbirth. While it is normal for new mothers to experience some level of emotional fluctuation due to hormonal changes, lack of sleep, and the overwhelming responsibility of caring for a newborn, postpartum depression is more severe and persistent. Unlike the “baby blues,” which typically resolve within two weeks, postpartum depression can last for months or even longer if left untreated.
What Differentiates Postpartum Depression from Baby Blues?
- Baby Blues: Mild mood swings, irritability, sadness, and anxiety that usually begin within the first few days after delivery and resolve within two weeks.
- Postpartum Depression: Intense feelings of sadness, hopelessness, and fatigue that interfere with daily functioning and persist for more than two weeks.
Causes of Postpartum Depression
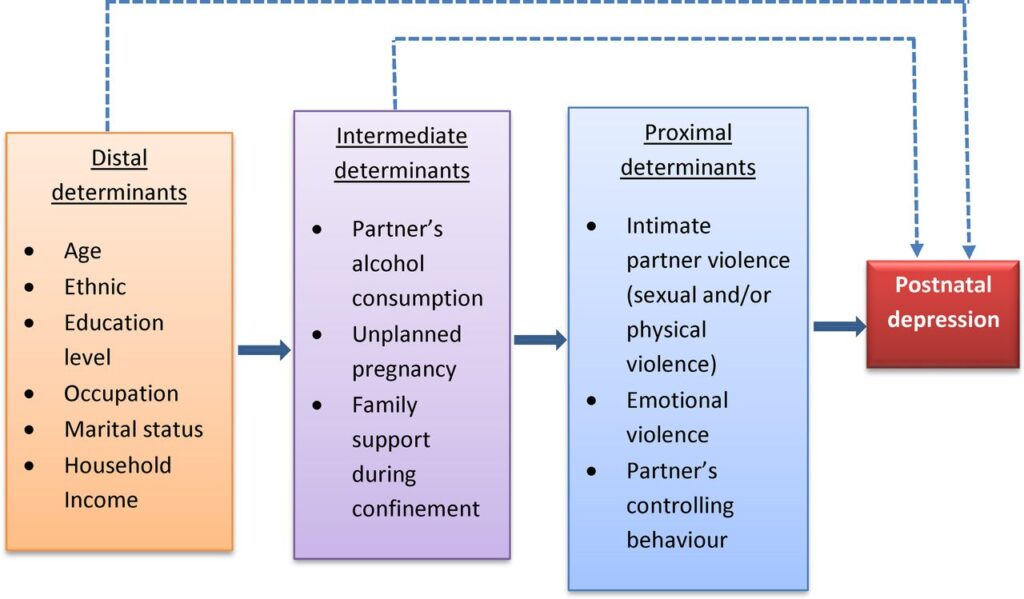
The exact cause of postpartum depression is not fully understood, but research suggests that it results from a combination of physical, emotional, and lifestyle factors. Below are some of the most common contributing factors:
Hormonal Changes
During pregnancy, levels of hormones such as estrogen and progesterone are significantly elevated. After childbirth, these hormone levels drop rapidly, which can lead to chemical imbalances in the brain. This sudden change may trigger depressive symptoms in some women.
Emotional Factors
The transition to motherhood can be emotionally overwhelming. Many women struggle with feelings of inadequacy, self-doubt, or fear about their ability to care for their newborn. Sleep deprivation and the stress of adapting to a new routine can also exacerbate these emotions.
Psychological History
Women with a history of depression, anxiety, or other mental health disorders are at a higher risk of developing postpartum depression. Similarly, those who have experienced postpartum depression in previous pregnancies are more likely to encounter it again.
Lifestyle Stressors
External factors such as financial difficulties, relationship problems, or a lack of social support can contribute to the development of postpartum depression. The absence of a strong support system can leave new mothers feeling isolated and overwhelmed.
Symptoms of Postpartum Depression
Recognizing the symptoms of postpartum depression is essential for timely intervention. These symptoms can vary in intensity and may include:
Emotional Symptoms
- Persistent feelings of sadness, emptiness, or hopelessness
- Frequent crying spells without an apparent reason
- Irritability, anger, or frustration
- Loss of interest in activities once enjoyed
- Feelings of worthlessness or guilt
Behavioral Symptoms
- Difficulty bonding with the baby
- Withdrawal from family and friends
- Neglecting personal care or household responsibilities
- Trouble concentrating or making decisions
Physical Symptoms
- Extreme fatigue or loss of energy
- Changes in appetite, leading to weight loss or gain
- Sleep disturbances, such as insomnia or excessive sleeping
- Unexplained physical aches and pains
Thoughts of Harm
In severe cases, women with postpartum depression may experience thoughts of harming themselves or their baby. This is a medical emergency, and immediate help should be sought.
Risk Factors for Postpartum Depression
Certain factors can increase the likelihood of developing postpartum depression. Understanding these risk factors can help in identifying women who may need additional support:
- A personal or family history of depression or anxiety
- Experiencing stressful life events during pregnancy or after childbirth
- Having a difficult or traumatic childbirth experience
- Lack of emotional or financial support from a partner or family
- Being a young mother or having an unplanned pregnancy
- Having a baby with special needs or health complications
Care and Treatment Options
Postpartum depression is treatable, and early intervention can make a significant difference in recovery. A combination of therapies and support systems is often the most effective approach.
Professional Support
Seeking professional help is crucial for managing postpartum depression. Mental health professionals, such as therapists and psychiatrists, can provide guidance and treatment tailored to individual needs.
- Therapy: Cognitive-behavioral therapy and interpersonal therapy are commonly used to address negative thought patterns and improve communication skills.
- Medication: Antidepressants may be prescribed to help balance chemicals in the brain. It is important to discuss the risks and benefits of medication, especially if breastfeeding.
Support Groups
Joining a support group can provide a sense of community and understanding. Sharing experiences with other mothers who are going through similar challenges can reduce feelings of isolation and offer practical advice.
Lifestyle Adjustments
Making certain lifestyle changes can also aid in recovery:
- Rest and Sleep: Prioritize rest and seek help with nighttime feedings if possible.
- Nutrition: Maintain a balanced diet to support physical and mental well-being.
- Exercise: Engage in light physical activity, such as walking, to boost mood and energy levels.
Family and Social Support
Having a strong support system is vital for recovery. Partners, family members, and friends can play an active role by offering emotional support, helping with household chores, and providing childcare when needed.
Alternative Therapies
Some women find relief through alternative therapies, such as acupuncture, massage, or mindfulness practices like meditation and yoga. While these methods should not replace professional treatment, they can complement traditional approaches.
Preventing Postpartum Depression
While it may not always be possible to prevent postpartum depression, there are steps women can take to reduce their risk:
- Educate yourself about postpartum depression before giving birth.
- Build a support network of family, friends, and healthcare providers.
- Communicate openly with your partner about expectations and concerns.
- Take time for self-care and prioritize your mental health.
- Seek help early if you notice signs of depression or anxiety.
When to Seek Help
If you or someone you know is experiencing symptoms of postpartum depression, it is important to seek help as soon as possible. Early intervention can prevent the condition from worsening and ensure a healthier outcome for both the mother and the baby. Contact a healthcare provider, therapist, or helpline for guidance and support.