Pleurisy, also known as pleuritis, is a condition that affects the lining of the lungs and chest cavity. This inflammation can cause significant discomfort and may indicate an underlying health issue. Understanding what pleurisy is, its causes, symptoms, and available treatments can help individuals recognize the signs early and seek appropriate medical care.
What Is Pleurisy?
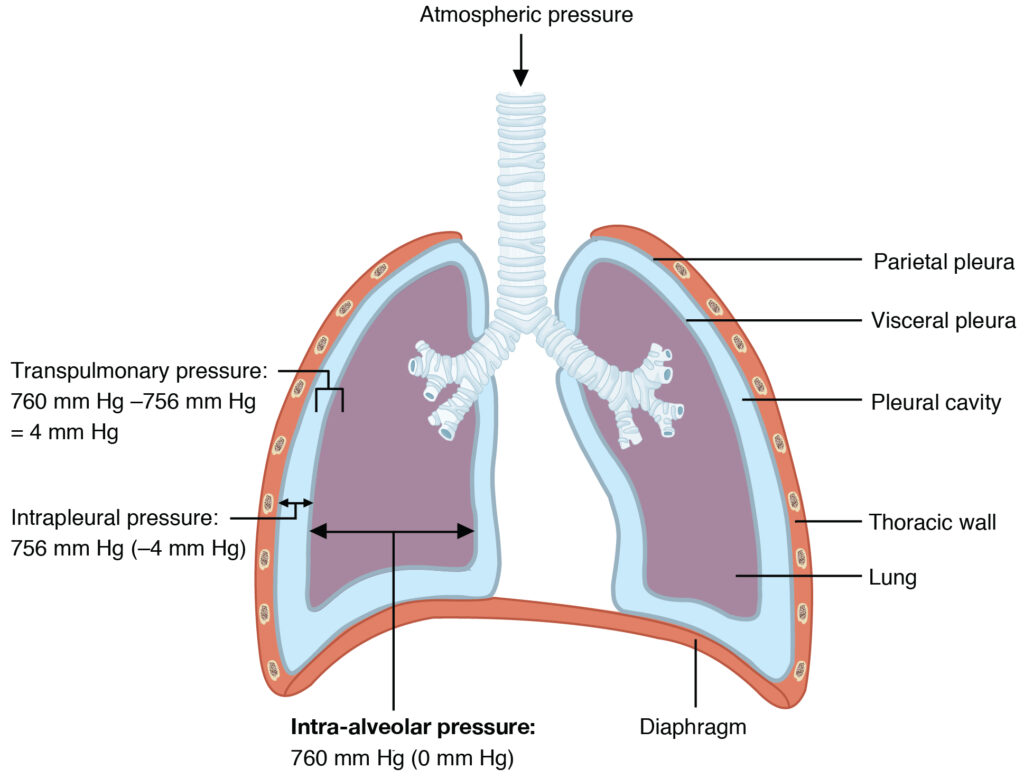
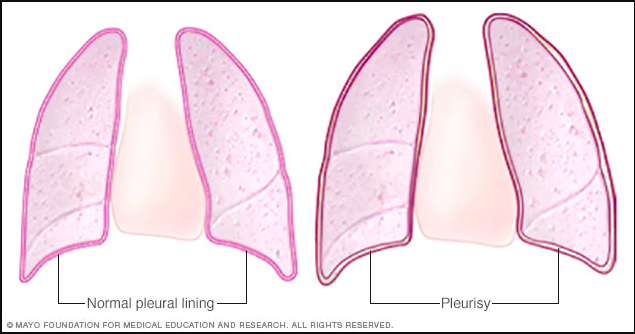
Pleurisy refers to the inflammation of the pleura, which is the double-layered membrane that surrounds the lungs and lines the chest cavity. The pleura helps reduce friction between the lungs and the chest wall during breathing. When this membrane becomes inflamed, it can lead to sharp chest pain and other symptoms. The condition often occurs as a result of an infection or another medical condition affecting the respiratory system.
How Does Pleurisy Affect the Body?
The primary function of the pleura is to facilitate smooth lung movement within the chest cavity. When the pleura becomes inflamed, its layers rub against each other, causing irritation and pain. This pain is typically exacerbated by deep breathing, coughing, or sneezing. In some cases, pleurisy can lead to the accumulation of excess fluid in the pleural space, a condition known as pleural effusion, which can further complicate breathing.
Causes of Pleurisy
Pleurisy can arise from a variety of causes, ranging from infections to autoimmune disorders. Below are some of the most common factors that contribute to the development of pleurisy:
Infections
- Viral Infections: Viral infections, such as the flu or other respiratory viruses, are among the most frequent causes of pleurisy. These infections can irritate the pleura, leading to inflammation.
- Bacterial Infections: Bacterial pneumonia is another common cause of pleurisy. The bacteria responsible for pneumonia can spread to the pleura, causing inflammation and pain.
- Fungal Infections: Although less common, fungal infections can also lead to pleurisy, particularly in individuals with weakened immune systems.
Lung Conditions
- Pulmonary Embolism: A pulmonary embolism occurs when a blood clot travels to the lungs, potentially causing inflammation of the pleura.
- Lung Cancer: Certain types of lung cancer can irritate the pleura, leading to pleurisy.
- Tuberculosis: Tuberculosis is a bacterial infection that primarily affects the lungs but can also cause pleurisy as a complication.
Autoimmune Disorders
- Rheumatoid Arthritis: This chronic inflammatory disorder can affect multiple joints and organs, including the pleura.
- Lupus: Systemic lupus erythematosus is an autoimmune disease that can cause widespread inflammation, including in the pleura.
- Scleroderma: Scleroderma is a condition characterized by the hardening and tightening of the skin and connective tissues, which can also affect the pleura.
Other Causes
- Chest Injuries: Trauma to the chest, such as from a car accident or fall, can damage the pleura and lead to inflammation.
- Certain Medications: Some medications, such as those used to treat heart conditions or cancer, can cause pleurisy as a side effect.
- Kidney Failure: Uremia, a condition associated with kidney failure, can lead to the accumulation of waste products in the blood, which may irritate the pleura.
Symptoms of Pleurisy
The symptoms of pleurisy can vary depending on the underlying cause and the severity of the inflammation. However, there are several hallmark signs that individuals should be aware of:
Chest Pain
Chest pain is the most prominent symptom of pleurisy. The pain is often described as sharp or stabbing and tends to worsen with deep breaths, coughing, or sneezing. In some cases, the pain may radiate to the shoulder or back. Unlike heart-related chest pain, pleuritic chest pain typically improves when the individual holds their breath or applies pressure to the painful area.
Shortness of Breath
Shortness of breath is another common symptom of pleurisy. As the pleura becomes inflamed, it can make breathing more difficult. If pleural effusion develops, the excess fluid can further restrict lung expansion, exacerbating the feeling of breathlessness.
Cough
A dry cough is often present in individuals with pleurisy. In some cases, the cough may produce sputum, especially if the underlying cause is an infection such as pneumonia or tuberculosis.
Fever and Chills
Fever and chills are frequently associated with infectious causes of pleurisy, such as viral or bacterial infections. These symptoms indicate that the body is fighting off an infection.
Other Symptoms
- Fatigue: Many individuals with pleurisy experience fatigue due to the body’s immune response and the effort required to breathe comfortably.
- Rapid Breathing: Rapid, shallow breathing may occur as the body attempts to compensate for the discomfort caused by deep breaths.
- Loss of Appetite: Some individuals may experience a decreased appetite, particularly if the underlying cause is an infection or systemic illness.
Diagnosis of Pleurisy
To diagnose pleurisy, healthcare providers rely on a combination of medical history, physical examination, and diagnostic tests. Proper diagnosis is essential to identify the underlying cause and determine the most effective treatment plan.
Medical History and Physical Examination
During the initial consultation, the healthcare provider will ask about the individual’s symptoms, including the nature and duration of the chest pain, any associated symptoms, and potential risk factors. A thorough physical examination will also be conducted, focusing on listening to the lungs with a stethoscope. A characteristic “pleural friction rub” may be heard, which is a grating sound caused by the inflamed pleura rubbing together.
Imaging Tests
- Chest X-ray: A chest X-ray can help identify abnormalities such as fluid accumulation or signs of infection in the lungs.
- Computed Tomography (CT) Scan: A CT scan provides more detailed images of the chest and can help detect underlying conditions such as tumors or blood clots.
- Ultrasound: An ultrasound of the chest can help visualize pleural effusion and guide procedures such as thoracentesis, where fluid is removed for analysis.
Laboratory Tests
- Blood Tests: Blood tests can help identify signs of infection, inflammation, or autoimmune disorders.
- Analysis of Pleural Fluid: If pleural effusion is present, a sample of the fluid may be collected and analyzed to determine its composition and identify potential pathogens.
Treatment Options for Pleurisy
The treatment of pleurisy depends on the underlying cause and the severity of the symptoms. While some cases resolve on their own, others require targeted interventions to address the root cause and alleviate discomfort.
Treating the Underlying Cause
The first step in treating pleurisy is addressing the underlying condition. For example:
- Infections: Antibiotics are prescribed for bacterial infections, while antiviral medications may be used for viral infections. Antifungal drugs are administered for fungal infections.
- Autoimmune Disorders: Immunosuppressive medications or corticosteroids may be used to manage autoimmune conditions such as rheumatoid arthritis or lupus.
- Pulmonary Embolism: Blood thinners are typically prescribed to prevent further clot formation and allow the existing clot to dissolve.
Pain Management
Pain relief is a key component of pleurisy treatment. Over-the-counter pain relievers, such as ibuprofen or acetaminophen, are often recommended to reduce inflammation and alleviate discomfort. In severe cases, prescription pain medications may be necessary.
Managing Pleural Effusion
If pleural effusion is present, additional measures may be required to remove the excess fluid and improve breathing. These include:
- Thoracentesis: This procedure involves inserting a needle into the pleural space to drain the fluid.
- Pleurodesis: In recurrent cases of pleural effusion, a chemical agent may be introduced into the pleural space to prevent further fluid buildup.
Lifestyle Modifications
Certain lifestyle changes can help individuals manage pleurisy and promote recovery:
- Rest: Adequate rest is essential to allow the body to heal and recover.
- Hydration: Staying well-hydrated can help thin mucus and ease breathing.
- Avoiding Irritants: Smoking and exposure to pollutants should be avoided, as they can worsen respiratory symptoms.
When to Seek Medical Attention
While mild cases of pleurisy may resolve without medical intervention, certain symptoms warrant immediate medical attention. These include:
- Severe or worsening chest pain
- Difficulty breathing or shortness of breath at rest
- High fever or chills
- Coughing up blood
- Signs of infection, such as redness, swelling, or warmth around the chest area
Prompt evaluation and treatment are crucial to prevent complications and ensure a favorable outcome.